Introduction
South Africa is one of the 15 Southern African Development Community (SADC) member states, one of the 55 member states of the African Union (AU), and one of the 47 WHO African Region (WAFR) member states.1 In 2022, the country had an estimated population of 60,731,936,2 a total gross domestic product (GDP) of International Dollars (Int$)904.743 billion, and a GDP per capita of Int$14,722.177.3 The country is an upper-middle-income economy with a human development index (HDI) of 0.705, an inequality-adjusted HDI of 0.463 and a Gini index of 63.0.4 The poorest 40% of the population hold 7.2% of national income compared to 50.5% and 19.2% of the wealthiest 10% and 1% of the population. The International Monetary Fund [IMF] projected that South Africa’s real GDP growth would shrink by -5.8% in 2020 due to coronavirus disease (COVID-19).5
Worldwide, there were a total of 531,750,839 coronavirus disease (COVID-19) cases as of 30 May 2022, which comprised 6,311,029 deaths and 502,670,865 recovered cases, and 22,768,945 active cases.2 By 30 May 2022, South Africa had conducted a total of 25,231,997 COVID-19 tests that revealed a total of 3,953,967 COVID-19 cases, which consisted of 101,146 deaths (2.6%), 3,803,725 (96.2%) recovered cases, and 49,096 (1.2%) active cases.2 These translated into 415,465 COVID-19 tests per million population, 65,105 cases per million population, and 1,665 total deaths per million population. In Africa, South Africa had the fifth-largest density of tests per million population, after Eswatini (868,115), Botswana (830,020), Cabo Verde (706,600), and Gabon (685,988).
South Africa recorded the highest burden of total COVID-19 in the African continent in terms of total cases and deaths per million population,2 which might be attributed to at least five factors. First, Wojcicki6 attributes it to the "… historically high frequency of travel between Europe and Republic of South Africa,…, it is possible there were more introductions of the virus in February and March compared with other sub-Saharan African countries (p.196)". The second factor is related to the high levels of poverty and unemployment. For example, in 2018, about 28% of the total labour force was unemployed,3 while 3,745,286 people (6.3% of the population) lived in multidimensional poverty.4 According to Karim,7 “Poverty and unemployment mean many people live in informal settlements where implementing preventive interventions such as hand washing, and social distancing is difficult” (p.e95(1)).
Third, as shown in Table 1, the country has a sub-optimally performing
national health system that might be associated with issues related to
health workforce,8,9 medical devices,10 infrastructure,10,11 and health expenditure. As a result, in 2019, South Africa had an average universal health service coverage index (UHC SCI) of 67 (on a scale of 0 to a target of 100), signifying an essential health services coverage gap of 33.12,13 That overall coverage deficit was due to gaps of 24, 32, 50, and 20 in the underlying UHC SCI components of reproductive, maternal, newborn and child health (RMNCH); infectious diseases (IDS); non-communicable diseases (NCH); and service capacity and access (SCA). The UHC SCI for South Africa was 21% higher than the WAFR score of 46.
Fourth, in 2019, about 81.06% of South Africa’s population used safely managed drinking water services; and 44.37% used a hand-washing facility with soap and water.11–13 Thus, 11,502,629 of the population were not using safely managed drinking water services; and 33,785,176 were not using a hand-washing facility with soap and water. Such people may have significant challenges in practising personal hygiene to prevent COVID-19 infection.
Fifth, to facilitate annual reporting as required by the 2005 World Health Assembly Resolution,15,16 the International Health Regulations (IHR) Secretariat developed a data collection tool used by each Member State to provide standardised information on progress in the development of 13 core IHR capacities.17 For example, in 2020, the World Health Organization reported that South Africa’s average of 13 International Health Regulations (IHR) core capacity score was 79 (on a scale of 0 to a target of 100), signifying a gap of 21%.18
As depicted in Table 2, out of 13 core IHR capacities in South Africa, only legislation and financing, laboratory, risk communication, radiation emergencies, and food safety had a target score of 100.18 The IHR capacity of the national health emergency framework had a gap of 53; human resources, points of entry, and zoonotic events and the human-animal interface each had a gap of 40; coordination and IHR national focal point functions and health service provision had a gap of 27; surveillance and chemical events had a gap of 20. Deficits in eight IHR capacities may have hampered South Africa’s efforts to mount a coordinated fight against COVID-19; screen for COVID-19 at all points of entry; perform testing, contact tracing, plus quarantine suspected cases; and isolate and effectively manage positive patients.19
Sixth, according to McIntyre, Meheus and Røttingen,20 “…a target of government spending on health of at least 5% of GDP [is needed] for progressing towards UHC” (p.125). Unfortunately, in 2019, South Africa’s domestic general government health expenditure was 4.9% of GDP14; thus, the need to continue advocacy for increased budgetary allocations.
There is a shortage of evidence on the economic value of human life losses associated with COVID-19 in Africa, although such information is needed for evidence-based advocacy. Such evidence has been generated in Brazil,21 Canada,22 China,23 France,24 Germany,25 India,26 Iran,27 Italy,28 Japan,29 Mauritius,3 Spain,30 Turkey,31 the United Kingdom,32 and the United States of America,33 for use in advocacy for increased investments into health-related systems in pursuit of the United Nations Sustainable Development Goal 3 on “Ensure healthy lives and promote wellbeing for all at all ages” (p.14).34
To date, no study has attempted to estimate the present (or discounted) economic value of human life losses associated with COVID-19 in South Africa. This study contributes to bridging that information gap. This study estimated the total present value of human life (TPVHL) losses associated with COVID-19 in South Africa as of 30 May 2022.
Material and methods
Study location and design
The study reported in this paper was conducted in South Africa and used a cross-sectional design. It was based on the entire population of 101,146 people reported having died from COVID-19 in South Africa by 30 May 2022.2 That is the cumulative number of deaths reported between 5 March 2020, when the first case of COVID-19 was confirmed and 30 May 2022.35
Conceptual framework
Mooney describes and exhaustively critiques the three competing methods of valuing human life monetarily, i.e., the willingness to pay approach (WTP), the implied values (revealed preference) approach (IVA),36 and the human capital approach (HCA). According to Jones-Lee,37 the WTP "…focuses upon the amount that individuals would be willing to pay, or would require in compensation, for variations in safety (minimal changes in the probability of death from a particular cause that will result if a particular public sector project (programme or intervention) is undertaken" (p. 143). Broome critiqued the application of WTP in eliciting people’s evaluations of probabilities of death from disease or injury but received a rebuttal from Jones-Lee.38,39 The WTP approach has been applied in Africa to elicit the maximum amount of money people would be willing to pay to prevent death from schistosomiasis,40 health insurance,41–44 treatment of tuberculosis,45 and malaria control.46,47
The HCA values human life as “…discounted expected future earnings stream net of his consumption” (p.427).48 Robinson traces the philosophical origins of the HCA valuation of life.49 The HCA has been applied in Africa to value human life losses associated with child illnesses,50 cholera,51 COVID-19,21–33,52 diabetes,53 Ebola virus disease,54 malaria,55 maternal disorders,56 neglected tropical diseases,57 non-communicable diseases,58 suicide,59 and tuberculosis.60 In the current study, the HCA was applied in the valuation of human life losses associated with COVID-19 due to the availability of relevant data on the number of COVID-19 deaths by age group, GDP per capita, current health expenditure per capita, and average life expectancy at birth.
Our study replicated the HCA methodology applied in various countries to monetarily value lives lost to COVID-19.21–33,52 The total present value of human life losses associated with COVID-19 in South Africa equals the sum of present values of human life losses in age groups 0-4 years, 5-9 years, 10-14 years, 15-19 years, 20-24 years, 25-29 years, 30-34 years, 35-39 years, 40-44 years, 45-49 years, 50-54 years, 55-59 years, 60-64 years, 65-69 years, 70-74 years, 75-79 years, and 80 years and older.
The formula can be expressed as:
TPVHLSouth Africa=j=17∑j=1VHLj
where: VHLj is the discounted value of human life losses from COVID-19 in jth age group; j=1 is group 0-4 years, 2=5-9 years, 3=10-14 years, 4=15-19 years, 5=20-24 years, 6=25-29 years, 7=30-34 years, 8=35-39 years, 9=40-44 years, 10=45-49 years, 11=50-54 years, 12=55-59 years, 13=60-64 years, 14=65-69 years, 15=70-74 years, 16=75-79 years, and 17=80 years and older; is the total of VHL across the seventeen age groups designated by integers 1 to 17.
The VHLj for each of the seventeen age groups was estimated with the following equation21–33,52:
VHLj=N∑n=1(1(1+1)n)×(R1−R2)×(R3−R4)×(R5×R6)
where: is the total from the year one of life lost (n=1) to the final year of life lost (N); R1 is the per capita GDP of South Africa in 2022; R2 is the per capita current health expenditure in South Africa in 2022; R3 is the average life expectancy at birth in South Africa; R4 is the average life expectancy at the onset of death from COVID-19 in jth age group; R5 is the cumulative number of COVID-19 deaths in South Africa by 30 May 2022; R6 is the share of COVID-19 deaths per age group.
Data and data sources
Several sources of data were used for the purposes of this study (Table 3).
Data analysis
We used Excel Software (Microsoft, New York) to estimate the human capital model consisting of two equations. The steps followed include:
Step 1: Estimating undiscounted years of life lost (YLL) per person who died of COVID-19 in a specific age group. It entailed subtracting the average age at the onset of death for a particular age group from South Africa’s average life expectancy at birth. Example: YLL for a person in the age group 0-4 years = South Africa’s average life expectancy of 64.88 years – the average age at onset of death of 2 years = 62.88 years. Thus, due to the scarcity of data, the average age of onset of death was a simple average of the age group.
Step 2: Estimating the discounted YLL per person who died of COVID-19 in a specific age group at a 3% discount rate. Each undiscounted YLL for the age group was multiplied by the relevant discount factor from the standard discount factor formula The first YLL = = 0.970873786; second YLL = =0.942595909; …; eightieth YLL = = 0.15533.
Step 3: Calculation of the net GDP per capita (NGPC) by subtracting South Africa’s current health expenditure per capita (CHEPC) from the GDP per capita (GPC). Thus, NGPC = GPC – CHEPC = Int$14,722.177 - Int$1,321 = Int$13,401.18 per person.
Step 4: Sharing COVID-19 deaths across seventeen age groups by multiplying the total COVID-19 deaths in South Africa reported on 30 May 2022 by an age group proportion.
Step 5: Estimating the total discounted economic value of human lives lost from COVID-19 per age group The for 0-4-year-olds equals the total discounted YLL per person (28.15567) in the age group times NGPC (Int$13,401.18) times the number of COVID-19 deaths in the age group (273.69). That is: Int$103,268,492.
Step 6: Sharing the total discounted economic value of total human lives lost from cumulative COVID-19 deaths reported on 30 May 2022 (TPVHL) across the seven administrative provinces in South Africa. The VHL was multiplied by the proportion of COVID-19 deaths incurred by each province.62
Step 7: Sensitivity analysis: The human capital model was re-calculated four times, assuming (a) 5% and 10% discount rates,21–33,50–60 and (b) the continental highest average life expectancy of 78.76 years (Algeria women) and the world highest life expectancy of 88.17 years (Hong Kong women) with all other parameters held constant.61
Results
The 101,146 human life losses associated with COVID-19 had a total present value of Int$7,566,656,063 and an average of Int$74,809.25 per human life (Table 4).
Approximately, 1.4% of the total present value of human lives lost accrued to 0-4-year-olds, 0.8% to 5-9-year-olds, 0.8% to 10-14-year-olds, 1.7% to 15-19-year-olds, 2.5% to 20-24-year-olds, 4.3% to 25-29-year-olds, 7.7% to 30-34-year-olds, 11% to 35-39-year-olds, 13.5% to 40-44-year-olds, 16.2% to 45-49-year-olds, 17% to 50-54-year-olds, 15.9% to 55-59-year-olds, 7.2% to 60-64-year-olds, and 0% to 65-year-olds and above. Ninety-seven percent (97%) of the total present value of human lives lost was borne by the most productive age bracket of 15-64 years. The average present value per human life declines as age increases. For instance, the present value per human life lost among 0-4-year-olds was ten-fold lower than that of 60-64-year-olds.
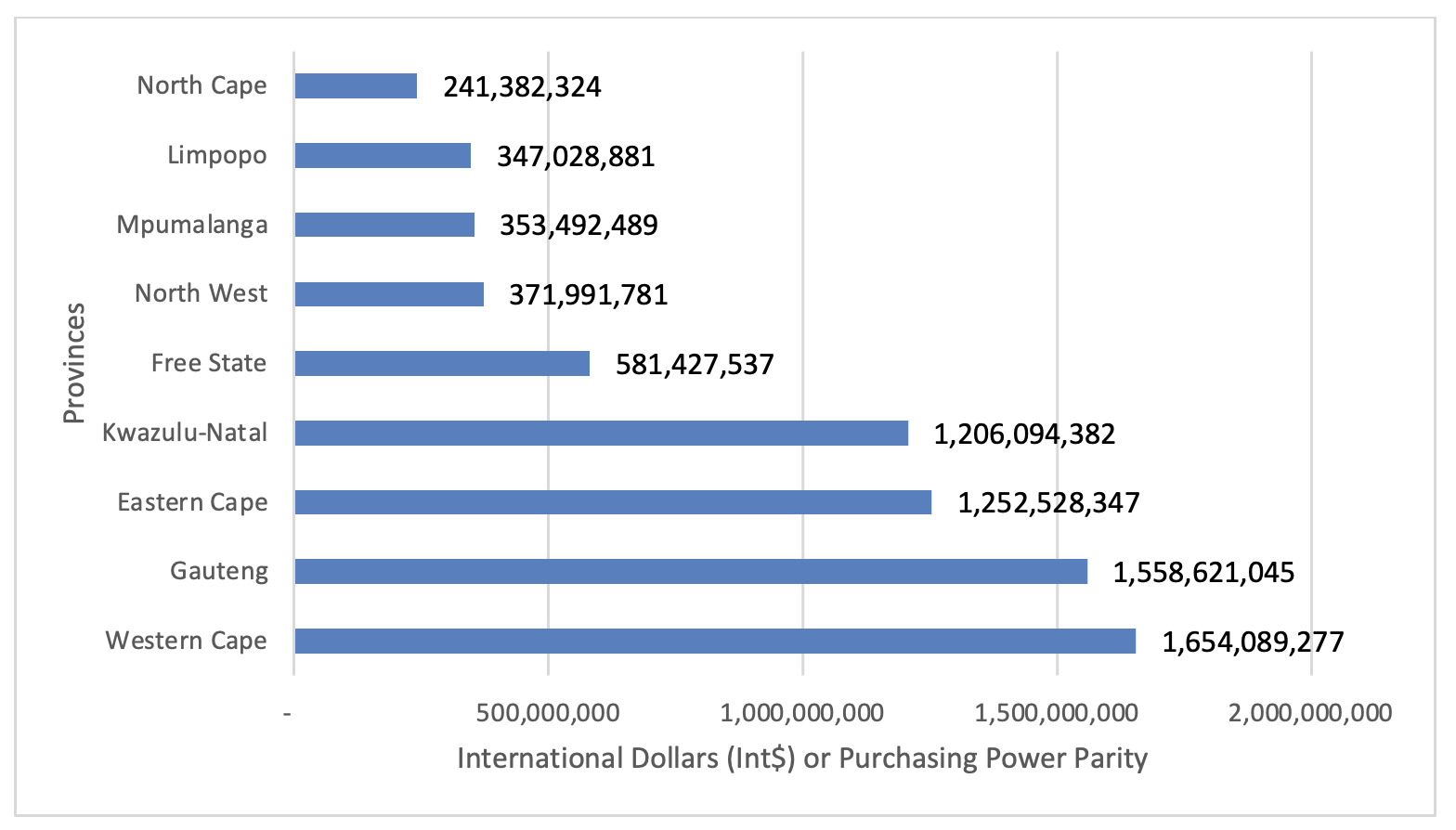
As depicted in Figure 1, 21.9% of the total present value of human lives lost accrued to Western Cape, 20.6% to Gauteng, 16.5% to Eastern Cape, 15.9% to Kwazulu-Natal, 7.7% to Free State, 4.9% to Northwest, 4.7% to Mpumalanga, 4.6% to Limpopo, and 3.2% to North Cape. About 75% of the total present value of human lives lost accrued to Western Cape, Gauteng, Eastern Cape, and Kwazulu-Natal provinces.
As depicted in Table 5, re-calculation of the human capital model alternately with 5% and 10% discount rates diminished the TPVHL by Int$1,177,446,403 (15.6%) and Int$ 2,997,459,371 (39.6%), respectively. The reductions in TPVHL translated into decreases of Int$11,641 and Int$29,635 in the average present value per human life lost.
As revealed in Table 6, the substitution of South Africa’s national life expectancy of 64.88 years with Africa’s highest average life expectancy (Algeria’s women) and the world’s highest life expectancy (Hong Kong women) of 78.8 years and 88.17 years triggered a growth in the TPVHL of Int$8,846,142,813 (117%) and Int$15,363,165,669 (203%), respectively. In turn, the mean TPVHL per human life grew by Int$87,459 and Int$151,891.
Discussion
This paper estimates the value of human life losses associated with COVID-19 in South Africa between 5 March 2020 and 30 May 2022. It has four key findings. First, the 101,146 human life losses associated with COVID-19 had a total present value of Int$ 7,566,656,063; that is 0.84% of South Africa’s total GDP in 2022. Second, the average present value per human life of Int$74,809 is five-fold the GDP per capita for South Africa in 2022. Third, re-calculating the human capital model with 5% and 10% discount rates diminished the total present value by 15.6% and 39.6%, respectively. Fourth, a rerun of the human capital model with Africa’s highest average life expectancy of 78.8 years and the world’s highest life expectancy of 88.17 years grew the TPVHL by 117% and 203%, respectively.
Donaldson and Mitton discuss the apparent absence of health economics in important debates surrounding COVID-19.63 Globally, there is a scarcity of studies on the monetary valuation of human life losses associated with COVID-19. For example, as shown in Table 7 below, the average present value per human life for South Africa of Int$74,809 is less than those of Spain by approximately 6-fold, Italy by 5-fold, China by 5-fold, France by 5-fold, Mauritius by 4-fold, United States of America (USA) by 4, Japan by 4-fold, Canada by 3-fold, Turkey by 3-fold, United Kingdom (UK) by 3-fold, Germany by 2-fold, Iran by 2-fold, Brazil by 1-fold, and India by 1-fold (Table 7).
Generally, the lower average present value per human life for South Africa might be attributed to the larger GDP per capita and longer average life expectancies in the comparator countries. For instance, the GDP per capita for South Africa of Int$14,722 in 2022 is lower than those of the USA by 5-times; Canada, France, Germany, and the UK by 4-times; Italy, Japan, and Spain by 3-times; Mauritius and Turkey by 2-times; Brazil and China by slightly above 1-times. However, even though the average value per human life in India and Iran was greater than that of South Africa, the latter had a slightly larger GDP per capita. Furthermore, the average life expectancy at birth for South Africa of 64.88 years was lower than those of Japan by 20 years, Italy by 19 years, Spain by 19 years, France by 18 years, Canada by 18 years, Germany by 17 years, the United Kingdom by 17 years, the United States of America by 14 years, Turkey by 14 years, China by 13 years, Iran by 12 years, Brazil by 12 years, Mauritius by 11 years, and India by six years.61
This paper presents evidence of the total and average present value of human life losses associated with COVID-19 in South Africa as of 30 May 2022. South Africa’s Department of Health and health development partners can use this economic evidence in conjunction with arguments of the United Nations [UN] International Bill of Human Rights to life (Article 03) and to services for meeting basic needs (food, clothing, housing, health care, and social security) (Article 25),64 to reinforce the case for augmenting investments into South Africa’s national health system, disease surveillance and response system, and other systems that address social determinants of health. Furthermore, increased investments are needed to bridge extant gaps in the coverage of essential health services, water and sanitation services, and International Health Regulations core capacities to eradicate the ongoing COVID-19 pandemic and to mitigate and respond to future public health emergencies of national and international importance.
This study has a few limitations. First, the human capital approach has been criticised for discriminating against the lives and societal contributions of those outside formal market production. The standard human capital approach would value at zero potential years of life losses accruing to children below the minimum work-age limit, homemakers, unemployed, retired, and those who cannot work due to handicaps.65,66 Also, it has been criticised for ignoring a person’s perceptions of their welfare67 and for assuming that the only objective of saving human lives is to ensure the return to work.36 To avoid contravening Article 3 of the UN International Bill of Rights – which states “Everyone has the right to life, liberty and the security of person” (p.2)67 – the current study valued the YLL lost at all ages due to COVID-19 at the same per capita GDP net of current health spending per person.
Second, the GDP per capita used in the monetary valuation of human lives lost to COVID-19 ignores income and wealth inequalities, environmental degradation due to economic production processes, and wellbeing (quality of life).68 Third, the GDP per capita does not reflect differences in human capital due to variations in innate ability, schooling, school quality and non-schooling investments, pre-labour market peer group influences, and on-job training.69
Third, Wang et al. estimated that the reported COVID-19 mortality rate in South Africa had been underestimated three-fold.70 The authors attributed underestimation to “… underdiagnosis due to insufficient testing, reporting challenges, or higher than expected mortality from other diseases due to pandemic related changes in behaviours or reduced access to health care or other essential services (p. 1514)”. The underestimation of COVID-19 mortality implies that our reported estimates of the total present value of lost human lives are also likely to underestimate.
Fourth, as reported by WHO, UNICEF and IFRC,71 COVID-19 patients, family, friends, and caregivers are labelled, stereotyped, and discriminated against, leading to erosion of their social wellbeing. Family members and friends of those who die from COVID-19 also experience psychological pain due to losing their loved ones. Since our study did not quantify these indirect adverse effects, it may have contributed to further underestimation of the actual effect.
Fifth, alternative valuation methods, instead of the HCA, might yield different value of life estimates. For example, Hirth et al. review of the published value of life literature found the median value of a quality-adjusted-life-year (QALY) to be US$24,777 (from HCA studies), US$93,402 (from revealed preference/non-occupational safety), US$161,305 (from WTP studies), and $428,286 (from revealed preference/job risk studies),72 implying that a human life lost due to COVID-19 might be worth much more than our HCA estimate.
Conclusion
This paper’s primary purpose was to estimate the present value of human life lost due to COVID-related mortality in South Africa. This study has revealed that COVID inflicted a significant human toll on South Africa. Each human life lost from COVID-19 in South Africa had an average present value of Int$74,809, five-fold the GDP per capita for South Africa in 2022, setting the country back a few years in terms of socio-economic development. This finding implies the need to campaign within the South African Government for increased investments in strengthening health-related systems to curtail human life and economic losses from the ongoing pandemic and mitigate losses from similar public health emergencies.
The current study did not estimate the cost and benefits of alternative prevention and control interventions for COVID-19. Therefore, the evidence contained in this paper is meant exclusively for use in awareness-raising and public health advocacy. There is a need for a cost-benefit analysis of all possible prevention, management, and rehabilitative interventions for the disease to guide multi-sectoral policy development and decision-making around COVID-19.
Acknowledgements
The authors owe profound gratitude to Jehovah Jireh for inspiration and sustenance during the study process. The paper is dedicated to all health workers (past and present) worldwide for the gallant public health war against COVID-19. The views expressed in this paper are entirely those of the authors and should not be attributed to institutions of affiliation.
Author contributions
JMK, GMM, and FM contributed to the literature review, data extraction from various databases, conceptualisation, development of the human capital approach model on Microsoft Excel, formal analysis, findings interpretation, and manuscript writing. All authors approved the final version of the paper.
DECLARATION OF CONFLICTING INTERESTS
The authors completed the ICMJE Unified Competing Interest form (available upon request from the corresponding author) and declared no conflicts of interest.
ETHICAL APPROVAL AND CONSENT TO PARTICIPATE
The analysis relied entirely on the secondary data published in freely accessible international databases of the Worldometers, IMF, Republic of South Africa COVID-19 statistics, and WHO. Thus, ethical approval was not required.
FUNDING
The authors received no financial support for this paper’s research, authorship, and publication.
AVAILABILITY OF DATA AND MATERIALS
The secondary data analysed in this study are openly accessible from the following websites:
-
Covid-19 case data from Worldometers2:
https://www.worldometers.info/coronavirus/ -
GDP data from International Monetary Fund (IMF) World Economic Outlook Database3:
https://www.imf.org/en/Publications/WEO/weo-database/2021/October -
Average life expectancy data from Worldometers61:
https://www.worldometers.info/demographics/life-expectancy/#countries-ranked-by-life-expectancy -
Per capita current health expenditure data from World Health Organization (WHO) Global Health Expenditure Database14:
https://apps.who.int/nha/database/Select/Indicators/en
CORRESPONDENCE
Professor Joses Muthuri Kirigia, African Sustainable Development Research Consortium (ASDRC), PO Box 699400100, Nairobi, Kenya. Email: muthurijoses68@gmail.com.