Introduction
Awareness of the public health burden represented by road insecurity is a recent development. The highest accident rates with casualties globally were recorded in Africa (26.6 for 100,000 inhabitants); on a global scale, road traffic accidents are the ninth cause of mortality, whereas in Africa they surfaced on a high fifth place.1 The majority of deaths concern vulnerable groups (pedestrians, two-wheeled vehicle users) and young people (5-44 years); according to the WHO data, road accidents today represent the first cause of mortality in 14-29 year-olds, including those in low- or middle-income countries.1
The framework of the road accidents can be viewed from four perspectives: pre-hospital care, the emergency medical service (EMS), hospital care and post-hospital care. Some of the most important barriers in better understanding and consequently providing efficient interventions include the lack of organizational models, inexistent or inappropriate training centres, problems linked to the cost of care as well as sustainability, faced with the high demand for services.2 Although the emergency medical care managed to improve the health of the African populations over the past 20 years, the advances in the domain of road trauma remained modest.3,4
Recent data on road traffic accidents in Burkina Faso managed to provide some limited evidence for policy.5,6 A surveillance system of accidents and traumas, supplied in the field by the national police and the doctors of the university hospitals, made it possible to measure the importance of the phenomenon and highlighted the difficulties of emergency medical care appropriate to the needs of road traffic casualties.
The sustainable development goal 3.6 requires a 50% reduction in the number of injuries and deaths,7 which in adjunction with the next decade guideline for road safety defined at the last world summit of Stockholm in 2020,8 provide a solid framework for improvement. Therefore, the objective of this study was to perform the initial assessment by revision of available literature, interviews and monitoring visits regarding the road traffic casualties in Burkina Faso which, to our knowledge, does not exist neither here nor in other Sub-Saharan countries of Western Africa. The ultimate goal of this work is to enable a better understanding of the outstanding issues and challenges, providing direly needed evidence for policy towards meeting the challenges of the SDGs.
Methods
We carried out a situational analysis9,10 of the care of road traffic casualties. It was based on a review of available data and resources in Africa in general,11–13 and official documents related to road safety and traffic casualties in Burkina Faso.14,15 In addition, we performed monitoring visits and observations at every stage of care. An inventory of the provision was made during monitoring visits, collecting the relevant data that accompanied the most obvious research gaps in knowledge. We also interviewed stakeholders from the following groups: Brigade Nationale des Sapeurs-Pompiers (the National Fire Brigade), the only pre-hospital patient care structure; by all the CHU (University Hospitals) in the country (n=5) and the two national hospitals of reference for hospital care and one CMA (Centre Médical avec Antenne Chirurgicale – Medical Centre with Surgical Unit). The analysis focused on the five central services in road trauma care, the Service d’Accueil des Urgences (SAU – Accident and Emergency – A & E), the orthopaedic-trauma department, the neurosurgery department, the visceral surgery department, and the intensive care unit. We also examined the data on functional rehabilitation units for post-hospital care, which was available in the public domain. In total, we interviewed 64 stakeholders, whose responses were compared with the existing norms for trauma victim care.14 We did not perform a complete qualitative study with these stakeholders, but only aimed to provide an overview of the current situation, giving rise to the most important research gaps that are required for the development of a holistic intervention plan.
Ethical autorization was given by the Comité d’éthique institutionnel pour la recherche en santé de l’Institut de Recherches en Sciences de la Santé (IRSS) of Burkina Faso (decision n° 08/2020 of 27 January 2020).
Results
Review of previously published studies
The overview of the available literature did not provide sufficient amount of evidence for our assessment. Although there were similar articles published for other African countries, we were not able to identify a relevant source for Burkina Faso. The grey literature and the official documents in Burkina Faso were also imprecise regarding the care provided to the injured. Only the statistical yearbooks show the number of patients cared for by the BNSP (National Fire Brigade) and CHU (University Hospitals),16 with a rather imprecise reference to accidents on the public highway. Similarly, the inventory of care provision and the capacities of care are dated and imprecise.17
Pre-hospital care
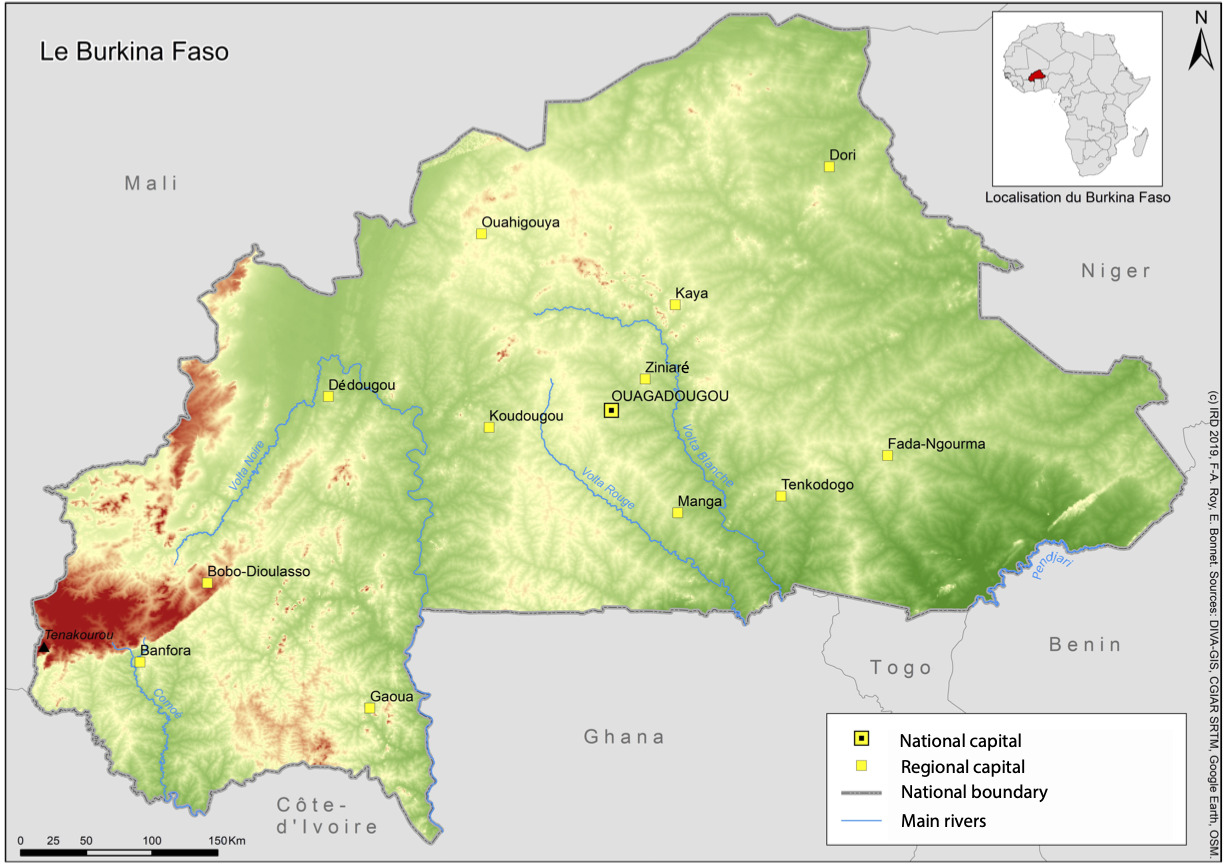
The Brigade Nationale des Sapeurs-Pompiers (BNSP – National Fire Brigade) is the main care provider for road casualties. Some partners further strengthen the pre-hospital care provision emergency response, like the Order of Malta and the Burkina Faso Red Cross at Bobo Dioulasso and Ouagadougou. The National Fire Brigade includes nine companies in the entire country, two of which are at Ouagadougou and one at Bobo-Dioulasso. It transports 80% of road casualties to care structures.5
The National Fire Brigade has recognized operations capacities, respect for protocols and a modern, functional call centre. It is, however, insufficiently established throughout the territory. The four centres in Ouagadougou and the two centres in Bobo seemed overburdened in the face of the rapid rise in urbanization and increased population density.
The latest studies in Ouagadougou suggested a very disappointing result, with a median 51-minute response between the call and the admission to accident and emergency care.18 The National Fire Brigade does not provide medical care on site, despite two military doctors being included in the National Fire Brigade staff. Furthermore, the National Fire Brigade’s companies do not seem to provide equal coverage across the country. This means that the majority of pre-hospital care is therefore undertaken by the next of kin or bystanders present at the crash scene, without proper medical assistance.
Hospital care - Services d’Accueil des Urgences (SAU – The Accident and Emergency departments) Infrastructures
Burkina Faso’s hospital care provision depends mainly on the public sector. This provision of care hinges upon the reference establishment in the final tier, which admits the biggest number of road casualties, including the four Centres Hospitaliers Universitaires (CHU – University Hospitals) of Ouagadougou and the University Hospital of Bobo Dioulasso.
At Ouagadougou, the Tengandogo University Hospital is more recent and comparatively more modern, with an appropriate layout of the A & E and resuscitation facilities. The inner organization however, could be further improved; out of the existing 24 cubicles in the resuscitation unit, six are used and only three are fully equipped (inventory assessment was performed before the COVID-19 epidemic).19
At the Bogodogo University Hospital, the A & E premises are relatively well laid-out and very spacious. The construction is recent, with one pharmacy and one standard radiology room incorporated within the emergency department. Eight intensive care cubicles are laid out in the A & E section dedicated to trauma emergencies. We managed to observe the efficient transfer of patients towards the orthopaedic unit during the visits.
The situation at the Yalgado Ouedraogo University Hospital, the national reference hospital, is the most concerning. The premises are dilapidated, insalubrious, under-equipped, and saturated. Patients are often asked to lie on the floor along corridors with very limited medical and paramedical monitoring. Equipment and amenities were in most cases damaged or defective. The neurosurgical department alone is maintained in a good state of operations, thanks to an active partnership between the Yalgado University Hospital and that of Clermont-Ferrand.20
The Charles De Gaulle University Hospital, the national reference hospital for paediatric emergencies, has all the emergency facilities in one place. This department is undersized as it is in heavy demand and often saturated. According to our observation, the infrastructures are adequate, but the equipment suffers from wear and tear and is sometimes defective.
At the Sanou Sourou University Hospital, the reference hospital for the entire western region of the country, the A & E department admitting surgical emergencies is located in a building distinct from that of medical emergencies; it adjoins the orthopaedic and traumatology department. It has a Service d’Accueil des Urgences vitales - SAUV (life-threatening accident and emergency unit) with two beds, and operational premises. The operating theatres for trauma and visceral emergencies are embedded in the A & E department together with a recovery room. According to the emergency physicians interviewed, the equipment is well-worn and sometimes defective.
On the whole, numerous shortcomings appeared with respect to A & E response to road casualties. In addition, no norms or national and international recommendations concerning life-threatening A & E currently exist in Burkina Faso.14
Organization of care
Medically-aided triage of the injured is not generally performed in all establishments. Organization of care is very separate (with the exception of A & E and traumatology) and is difficult to perform, as the triage of patients upstream is not carried out in concrete terms. During the monitoring visits, we observed the absence of care protocols that are written, mastered and applied by the staff in every establishment.
Quality of care and human resources
Aside from a generally poor opinion of A & E care for casualties on the part of users,21 it has been observed that the teams show little aptitude to manage absolute or life-threatening emergencies (multiple traumas, haemorrhagic shocks, etc.). The main reason is the absence of qualified emergency doctors and/or resuscitators. There are no senior doctors on call at A & E. The majority of patients are seen by trainee interns. A further difficulty is that there are no nurses specialized in emergency care in A & E departments.
Diagnostic tools, biomedical inputs and medical devices
Some biology laboratories within the university hospitals are not able to carry out all the necessary tests in continuous fashion and 24/7. Regarding imagery, ultrasound is only available in one sole A & E department in situ, but the A & E staff are not trained in emergency ultrasound procedures. Only one hospital has a functional scanner (Schiphra Hospital). MRI is unavailable in Burkina Faso. Medical kits sold in the hospitals are often incomplete, just like some pharmaceutical products which are indispensable for patient care (analgesics / analgesics class II and III; vasopressive amines; sedatives and curares; blood products are also often in short supply).
Post-hospital care
Rehabilitation, one of the Primary Health Care (PHC) components has struggled to emerge in Burkina Faso for want of human and financial resources. Yet medical rehabilitation needs are great, in particular with regard to road casualties. According to a survey conducted in 2012 on the epidemiological profile of physical disability in Burkina Faso,22 traumatic pathology represented 25% of activity in functional rehabilitation centres with the main cause being road accidents. Post-hospital care of victims presenting after-effects is principally provided by public and private sector physical medicine and functional rehabilitation services and notably the denominational sector. With modest technical support platforms, the care mechanism for rehabilitation includes two categories of structures. The public structures located in the university hospitals (n=5), and other public structures (n=2) located in other establishments, one in the Tenkodogo University Hospital (Centre-East Region) and the other at Ouagadougou (the CNAOB). Non-profit private structures also have rehabilitation technical platforms. They number 31 denominational or voluntary structures, and two private for profit structures. However, only 12 of them have the ability to make and/or repair orthopaedic equipment for the country as a whole.
Discussion
This study identified numerous obstacles to improving the road accident care in Burkina Faso. Expectedly, problems and barriers were observed in all levels of care. The problems originated in the first response layer, managed by the Emergency Medical Service (EMS), was which was already seen in other African countries.23 The general organization of workers and the availability of qualified staff to manage absolute emergencies are defective and have a direct impact on mortality or on the management of more demanding cases.24,25
One of the most urgent concerns is related to human resources, which are both lacking in number, but also in proper training and experience across every stage. There were also some problems in regulation and coordination between the health care and the Fire Brigade. One of the first actions should be better integration and improvement of the first line of response. Other African countries, like Ethiopia, have tried out the use of partnerships with international institutions; this has turned out to be an effective strategy to create equitable relations and build sustainable health systems which can serve as a model for other world health partnerships.26
There were also numerous problems in hospital care and rehabilitation that were observed and identified; the most apparent one was poor coordination and logistics. Rehabilitation, replacement and the general roll-out of imaging material are imperative throughout the whole country as well as the introduction of essential drugs in resuscitation and intensive care units. In effect, rehabilitation is not very effective and it is inequitably distributed throughout the territory. The need to set up infrastructures adapted to physical medicine and rehabilitation is primordial, according to stakeholders. It is considered indispensable to set them up in each secondary or tertiary health establishment at the very least. Similarly, the refurbishment of the CNAOB workshops in order to produce orthopaedic apparatus with advanced technologies would make it possible to reduce the dependence of Burkina Faso on the outside. Embedded rehabilitation is an important and necessary component of an effective traumatology system. Prospective studies should examine how a dedicated rehabilitation unit could affect the results in the medium and long term focused on the patient.27
Added to these shortcomings is a mechanism of pre-payment for tests and kits, which obliges users without financial means to find the necessary funds before seeking treatment. This constitutes a major barrier with respect to the quality of care because it causes delays in the diagnosis. There are major financial barriers for access to care in Burkina Faso and a great deal of research has shown the detrimental consequences for populations and most particularly the poorest.18 Implementation of public policies and the role of front-line actors (the police, health officials) with regard to their application remain central.28
Limitations
The study concerns only the establishments which provide emergency care to road casualties. It is therefore limited to the capital, Ouagadougou and Bobo-Dioulasso, the country’s second city. Yet there is a large number of casualties on the country’s rural roads far from these two cities. The CSPS (Health and social advancement centres) provide care in these conditions, despite not being equipped for this type of care. These CSPS (n=3320) were not visited during this study. Another limitation of this study is related to the methodological framework, which utilized available data and monitoring visits, but substantially lacked sufficient amount of primary and reliable studies. Most of the findings reported here are therefore possibly biased, but they do provide the initial step towards the development of a holistic intervention. Nevertheless, this study identified some of the most obvious gaps and therefore it provides an important collection of evidence available thus far.
Conclusion
This situational analysis of the care of road traffic casualties uncovers, therefore, many gaps in the Burkina Faso system. This example of Burkina Faso is revealing of low- and middle-income countries in Africa where integration of a basic level of medical emergency care in the health care systems could have a significant impact on the welfare of populations. The priority should be given to creating minimal directives for emergency medical care. This study identified numerous problems, which need to be further explored and quantified, before a more systematic intervention can be applied across the country, aiming to reduce the negative burden of road accidents.
Acknowledgments
The authors would like to thank all the persons questioned for their availability. They would also like to thank the GDRI Sud Trauma colleagues for their support and re-reading of the article.
Funding
The project is piloted by Expertise France with funding from the Ministère de l’Europe et des Affaires Étrangères Français au bénéfice du Ministère de la Santé du Burkina Faso.
Authorship contribution
JBGS, TC, YB conceived the study. E.B. contributed to survey design and data collection. JBGS, TC, Y.B., A.O, S.G, B.T. undertook data analysis with support from E.B. All authors contributed to the interpretation of the results. EB drafted the manuscript with contributions from all the authors. All the authors have read and agreed to the published version of the manuscript.
Competing interests
The authors completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf, and declare no conflicts of interest.
Correspondence
Emmanuel Bonnet, PhD ; IRD, UMR 215 Prodig, CNRS, Université Paris 1 Panthéon-Sorbonne, AgroParisTech, 5, cours des Humanités, Aubervilliers, France; emmanuel.bonnet@ird.fr