Adolescents and young women remain disproportionately vulnerable to HIV infection, especially in sub-Saharan Africa, where structural and social barriers persist. This study seeks to identify the factors associated with HIV infection among youth aged 15–24 in Kinshasa, Democratic Republic of Congo, to guide targeted prevention and care strategies.
Globally, an estimated 5 million young people are living with HIV, and 41% of new infections occur in this age group; equating to one new infection every 30 seconds.1 The burden is highest in the global south, where access to prevention and care remains limited.2 In sub-Saharan Africa, adolescent girls and young women account for 71% of youth living with HIV, compared to 64% globally.2 Stigma, gender inequality, and limited access to youth-friendly services exacerbate their vulnerability. Despite a 30% global decline in HIV-related deaths, adolescent mortality is rising in Africa, suggesting gaps in care and support.3 Only 10% of boys and 15% of girls aged 15–24 know their HIV status, reflecting low testing coverage.3
Recent systematic reviews highlight that bundled interventions, combining economic support and life skills, can reduce HIV risk among adolescents, but implementation remains uneven across contexts.1 In the Democratic Republic of Congo, HIV prevalence among youth is 0.8%, with higher incidence among males (1.0%) than females (0.5%).4 In Kinshasa, prevalence reaches 1.6%, driven by urban poverty, overcrowding, fragmented family structures, and misinformation. Biological and psychosocial transitions during adolescence, such as sexual initiation and identity formation, further increase exposure to risk behaviors.3
Despite existing interventions, more than half of new adult infections still occur among youth aged 15–24.5 This underscores the need for locally adapted, evidence-based strategies. However, few studies have examined the specific socio-cultural and structural factors influencing HIV vulnerability among adolescents in Kinshasa. This study aims to fill that gap by identifying key determinants of HIV infection in this population, to inform targeted prevention, testing, and care efforts.
II. METHODS
STUDY SETTING
Kinshasa, the capital of the Democratic Republic of Congo, has an estimated population of 17,032,300 in 2024, spread across 9,965 km². The city faces major public health challenges, including HIV/AIDS, malaria, and tuberculosis, compounded by poor infrastructure and an underfunded health system. Social and economic inequalities are pronounced, with widespread poverty and limited opportunities for youth. Stigma and discrimination remain prevalent, especially among vulnerable groups, underscoring the need for targeted adolescent health interventions.
STUDY DESIGN
This analytical cross-sectional study draws on secondary data collected by the National Adolescent Health Program (PNSA) and PATHFINDER from adolescents aged 15 to 24 in Kinshasa. The use of these data is justified by the only data available specifically focused on adolescent health in the DRC, providing targeted information not available in larger national surveys such as DHS or MICS.
SAMPLING
The study sample comprised 1,675 adolescents, including 853 boys and 822 girls. A three-stage probability sampling method was employed to ensure geographic and demographic representation:
-
Primary sampling units: Municipalities were selected by PATHFINDER based on programmatic priorities.
-
Secondary sampling units: Neighborhoods or health areas within selected municipalities were randomly drawn.
-
Tertiary sampling units: Households were selected using a systematic sampling interval within each chosen avenue.
-
In each selected avenue, one household with an eligible adolescent was surveyed.
-
Households were visited in a clockwise direction to maintain consistency.
-
Replacements were permitted in cases of absence or ineligibility.
-
Health areas and plots were randomly selected to reduce selection bias.
-
Sampling weights and clustering effects were incorporated into regression models to adjust for design effects.
Non-response rates were not documented, which may limit the generalizability of findings. However, the multi-stage design aimed to capture a diverse cross-section of adolescents across Kinshasa’s urban landscape
STUDY VARIABLES
This analysis explored a range of variables to assess factors associated with HIV infection among adolescents:
-
Sociodemographic characteristics: gender, age, marital status, education level, religion, occupation, and household composition.
-
Age grouping: adolescents were categorized into two groups—15–18 years and 19–24 years—based on biological and social criteria defined by the program.
-
HIV-related knowledge: included awareness of transmission modes, prevention methods, and access to testing services.
-
Knowledge assessment: responses were self-reported and evaluated as either sufficient or insufficient across key indicators; no stratification by knowledge level (low, medium, high) was applied.
-
HIV status: determined through serological testing, enhancing internal validity.
-
Limitations: behavioral risk factors such as sexual activity, condom use, and substance use were not included, limiting control for potential confounders.
-
Bias considerations: self-reported knowledge may be influenced by social desirability, affecting accuracy.
This variable framework allowed for a focused analysis of structural and informational determinants, though the absence of behavioral data presents limitations in interpreting risk exposure.
DATA COLLECTION AND PROCESSING
The original baseline study was designed to generate key indicators related to sexual and reproductive health among adolescents. Data were collected using a structured questionnaire encompassing seven thematic domains:
-
Sociodemographic characteristics
-
Maternal and child health
-
Sexual and reproductive health services
-
Sexually transmitted infections (STIs) and HIV
-
Gender-based violence
-
Post-abortion care
-
Adolescent pregnancy and family planning
Interviewers underwent standardized training to ensure consistency in data collection, and a pre-test was conducted to validate the reliability of the questionnaire. In total, 1,779 questionnaires were administered, reviewed for completeness, and systematically coded. Data entry was performed using Epi Data software, followed by rigorous cleaning procedures to identify and remove incomplete or inconsistent records. These steps helped enhance the overall quality and integrity of the dataset used for analysis
STATISTICAL ANALYSIS
Univariate analysis described the sample using absolute and relative frequencies and medians. Bivariate analysis explored associations using cross-tabulations and binary logistic regression. Multivariate logistic regression identified independent predictors of HIV status.
Variables with p-value <0.05 in bivariate analysis were selected and used for multivariate analysis.
Multicollinearity was assessed using variance inflation factors (VIF > 5 excluded). Missing data were addressed by listwise deletion.
Model diagnostics included the Hosmer-Lemeshow test.
All inferential analyses were performed at the 5% significance level.
ETHICAL CONSIDERATIONS
Ethical approval was obtained from the Ministry of Health’s ethics committee. Informed consent was secured from all participants, with parental assent for minors. Confidentiality was maintained through anonymization, and participants were informed of their rights and study purpose
RESULTS
Sociodemographic characteristics of adolescents aged 15 to 24 in the city of Kinshasa
This table reveals several key sociodemographic trends. The majority of participants are male (55.8%), and young people aged 19 to 24 predominate with 59.2%. The study shows that 93.6% of adolescents are single, while 60.6% are still in school. Regarding religion, 53.4% attend revivalist churches, and 74.6% of households have at least five people.
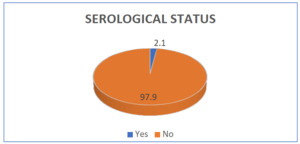
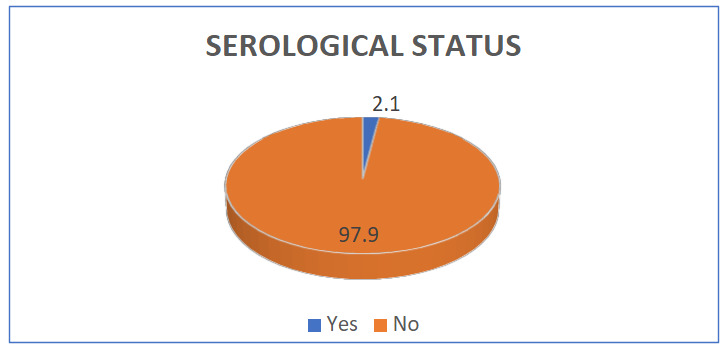
HIV prevalence among adolescents aged 15 to 24 in the city of Kinshasa
This figure shows that the prevalence of HIV among adolescents aged 15 to 24 in the city of Kinshasa is 2.1%.
Adolescents’ knowledge, perceptions and attitudes towards HIV
The results of this table reveal that the majority of adolescents, 99.4%, have already heard of HIV. Regarding sources of contamination, approximately 91.6% identify unprotected sexual intercourse as a major factor, while 84.0% mention the use of sharp objects. Regarding means of protection, approximately 81.0% consider the use of condoms as effective and 63.9% mention the avoidance of sharp objects.
This table reveals that the majority of adolescents surveyed (63.3%) know where to get tested, but only 24.8% have ever taken an HIV test. Of those who have been tested, 93.7% have collected their results. Testing is primarily initiated by health professionals (13.6%), while parents and partners play a minimal role in this decision. Finally, nearly 50% of adolescents report that their partner has already taken a test.
In this sample, nearly 75% of participants reported having no specific reason for HIV testing, indicating a low level of proactiveness. Prenatal care was cited by 1 in 10 people, while only 5% wanted to know their HIV status. Other motivations, such as awareness campaigns or medical reasons, remained marginal, indicating rather opportunistic testing.
Factors associated with HIV among adolescents aged 15 to 24 years in the City Province of Kinshasa
Bivariate analysis showed significant associations between HIV status and age, occupation, and knowledge of testing locations (p < 0.05). Adolescents aged 19–24 had 2.8 times higher odds of HIV positivity than those aged 15–18 (OR = 2.80; 95% CI: 1.22–6.44). Students were more likely to be HIV-positive than employed youth (OR = 2.26; 95% CI: 1.10–4.66). Knowing where to get tested was strongly protective (OR = 0.07; 95% CI: 0.01–0.52), highlighting the importance of access to information.
Among adolescents aged 15 to 24 years, in multivariate analysis, the results show that those aged 19 to 24 years are significantly more exposed to HIV than those aged 15–18 years (adjusted OR = 2.52; p = 0.032). Unemployed youth have a lower risk compared to those who work (OR = 0.34; p = 0.026). Significantly, students have a 4 times higher risk of being exposed to HIV, after adjustment (OR = 4.20; p = 0.004). In addition, knowing the testing location significantly reduces exposure to HIV, leading to a lower probability of being HIV-positive (OR = 0.08; p = 0.011).
III. DISCUSSION
KEY RESULTS
The study found that HIV positivity was significantly higher among adolescents aged 19–24 (2.8%) than those aged 15–18, likely due to increased autonomy and exposure, though behavioral data were lacking to confirm this. Students showed a four-fold higher risk compared to employed youth, possibly reflecting hidden vulnerabilities such as peer pressure or transactional sex. Unemployed adolescents had lower prevalence, potentially due to reduced mobility. Knowledge of testing locations was strongly protective (OR = 0.08), yet only 60% knew where to get tested, and testing remained largely reactive—70% had never been tested, and just 10% had done so in the past year. Despite high awareness of HIV and transmission modes, uptake of testing was low, suggesting that stigma, fear, and low perceived risk may hinder proactive behavior. These findings highlight the need for targeted, youth-friendly interventions and further qualitative research to explore underlying behavioral and structural factors.
HIV STATUS AMONG ADOLESCENTS IN KINSHASA
HIV prevalence among adolescents aged 15 to 24 in Kinshasa is estimated at 2.1%, higher than the national average of 0.8% reported in the 2013–2014 DHS.5,6 The National AIDS Control Program (PNLS) reported a national prevalence of 1.2% in 2020,7 confirming Kinshasa’s disproportionate burden. This elevated prevalence may be influenced by urban factors such as population density, informal settlements, and limited access to youth-friendly health services. However, the study lacks direct measures of urban risk environments, which limits causal interpretation.
Comparative data from other cities show variability: Kisangani (1.4%),8 Lubumbashi (1.7%),8 and Goma (3.4%).9 In Goma, higher prevalence may be linked to conflict-related displacement and increased vulnerability. These comparisons underscore the need for locally tailored interventions that account for regional dynamics, including mobility, conflict, and health infrastructure.
ADOLESCENTS’ KNOWLEDGE, PERCEPTIONS, AND ATTITUDES TOWARD HIV
While general awareness of HIV is high, testing behavior remains limited. Only 10% of adolescents had been tested in the past year, and 80% reported no specific reason for testing. Prenatal consultation was cited by just 10% as a motivator. This suggests that testing is often reactive rather than preventive, and that adolescents may not perceive themselves at risk. The lack of behavioral data prevents deeper analysis of risk perception.
In Kisangani, 45% of adolescents had ever been tested, and 8% in the past year.10 In Lubumbashi, 50% had been tested, with 30% citing antenatal consultations as a motivator.7 In Goma, 15% reported testing due to community campaigns.7,8 These findings highlight the impact of targeted outreach and integration of testing into routine services. Kinshasa’s lower proactive testing rates may reflect weaker community engagement or greater stigma.
Social stigma was identified as a barrier, but the dataset lacks qualitative insights to explore its manifestations. Future studies should incorporate interviews or focus groups to understand how stigma affects testing decisions, disclosure, and care-seeking behavior.
FACTORS ASSOCIATED WITH HIV AMONG ADOLESCENTS
Multivariate analysis identified age, occupation, and knowledge of testing sites as significant predictors of HIV status. Adolescents aged 19–24 were more likely to be HIV-positive (OR = 2.52; p = 0.032), likely due to increased exposure over time. Students had a higher risk than other groups, despite presumed access to information. This paradox suggests that information alone does not translate into protective behavior, and that student environments may harbor unique vulnerabilities.
Knowledge of testing locations was protective, yet testing rates remained low. This gap between awareness and action may be driven by fear of stigma, lack of confidentiality, or limited youth-friendly services. The study’s reliance on self-reported knowledge and absence of qualitative data limits the ability to fully interpret these dynamics.
In Goma, community campaigns led to higher testing rates (50%),11,12 demonstrating the effectiveness of proactive outreach. Couple testing, often initiated during medical events like prenatal consultations, also showed promise but remains circumstantial.13,14
To improve testing uptake, strategies must go beyond awareness. Integrating HIV screening into routine adolescent care, reducing stigma through peer-led education, and expanding youth-friendly services are essential. Future research should include behavioral and qualitative components to better understand the barriers and motivators influencing adolescent HIV risk and testing behavior
STRENGTHS AND LIMITATIONS OF THE STUDY
This study, based on a large adolescent sample in Kinshasa, offers valuable insights into HIV prevalence and associated factors using rigorous statistical methods. Its strengths include serological HIV testing and a multidimensional analysis of sociodemographic and informational variables. However, limitations include its cross-sectional design, reliance on self-reported data, absence of behavioral risk indicators, and geographic restriction to Kinshasa. These factors limit causal inference and generalizability. Despite these constraints, the study effectively identifies key vulnerabilities and supports the development of targeted, youth, focused HIV prevention and testing strategies.
CONCLUSION
This study reveals persistent gaps in HIV prevention and testing among adolescents in Kinshasa, despite high awareness levels. Testing remains largely reactive, underscoring the need for proactive education and accessible youth-friendly services. Age, education, and occupation shape vulnerability, demanding tailored interventions. Enhancing knowledge of testing sites could improve uptake and early detection. A comprehensive strategy, combining education, access, and stigma reduction is vital to curb HIV transmission in this population.
ACKNOWLEDGEMENTS
We thank the adolescents who participated in the study, the data collection team, and the study facilitator. We also acknowledge the Ethics Committee of the School of Public Health, University of Kinshasa, for its support. Their contributions were essential to the successful completion of this research.
DISCLAIMER
The views expressed in this manuscript are those of the authors and do not necessarily reflect the official position of Kinshasa University or any affiliated institutions.
ETHICS STATEMENT
This study received ethical approval from the Ethics Committee of the School of Public Health, University of Kinshasa (Approval No. ESP/CE/2025/014). Informed consent was obtained from all participants prior to data collection. For minors, consent was obtained from parents or legal guardians.
DATA AVAILABILITY
The data supporting the findings of this study are available from the corresponding author upon reasonable request.
FUNDING
This research received no external funding. The article publication charge (APC) was not funded by any third party.
AUTHORSHIP CONTRIBUTIONS
- Fernand LUENGA MAYAYA led the study design, data analysis, and manuscript drafting.
-
Bernard-Kennedy NKONGOLO contributed to data analysis, drafting, and revision.
-
Valery BIDUAYA, Hakim KADIMA, and Liévin TSHIMANGA supported manuscript editing.
-
MUSEMA MULAKILWA ALI Godefroid and Wivine KAVULA served as facilitators, providing oversight, academic guidance, and final validation.
DISCLOSURE OF INTEREST
The authors completed the ICMJE Disclosure of Interest Form (available upon request from the corresponding author) and disclose no relevant interests.