INTRODUCTION
While vaccination stands as one of the 20th century’s greatest public health achievements, its success has been consistently challenged by public concerns over vaccine safety, often leading to delays in acceptance or outright refusal. Healthcare workers (HCWs) occupy a unique and pivotal position; at the frontlines looking after patients and communities during the COVID-19 pandemic. They were confident in their knowledge, aware of infection risks,1 and often showed concerns about vaccine coverage.2 Moreover, their attitudes toward vaccination are particularly consequential, as they directly influence the perceptions of patients and the broader community, thereby shaping public trust in vaccination programs.3,4 In response to this global challenge, the World Federation of Public Health Associations (WFPHA) initiated a 12-country study to investigate the pandemic’s impact on HCW vaccine hesitancy (VH) and vaccine sentiment (VS).
VH is a complex and persistent issue5–7 defined by the WHO SAGE working group as a “delay in acceptance or refusal of vaccination despite availability of vaccination services.”8 Understanding the psychological determinants of VH is crucial, and the 5C model is a widely used framework for this purpose.9–13 According to this model, VH is driven by Confidence (trust in vaccine safety, efficacy, and the health system) and Collective Responsibility (the willingness to vaccinate to protect others).9,14–21 Conversely, it is hindered by Complacency (low perceived risk of disease), Constraints (structural barriers like access and affordability), and Calculation (extensive, effortful information seeking).11
Distinct from VH, which is an observable behavior, VS refers to the underlying attitudes, beliefs, and emotions that individuals and communities hold towards vaccines. These sentiments are a critical precursor to action, significantly influencing vaccination uptake and broader public health outcomes.22–25 Positive VS is generally associated with lower hesitancy and higher vaccination rates, and has also been linked to greater engagement with information from health authorities.22,26 Conversely, negative sentiments have been clearly linked to higher VH. In Brazil specifically, factors such as fear of side effects, distrust in the rapid pace of vaccine development, and exposure to misinformation have been identified as key drivers of hesitancy among HCWs.27
Understanding the context-specific determinants of VS is therefore crucial for improving public health outcomes and strengthening pandemic preparedness.3,16 This study contributes to this goal by analyzing data from the Brazilian arm of a broader international initiative.28 Accordingly, our primary objective is to explore the determinants of VS among Brazilian HCWs. Our five secondary research objectives (ROs), along with the corresponding analysis procedure for each, are detailed in Table 1.
Methods
2.1. Study Design
This research constituted a segment of a cross-sectional online self-administered survey,28 encompassing members from 12 national public health associations from Australia, Brazil, Canada, China, France, Germany, India, Italy, New Zealand, Spain, the UK, and the USA. The questionnaire development, dissemination, ethics approval, and general results of 12 countries were detailed in the prior publication,28 The questionnaire was uploaded onto SurveyMonkey and administered from the 14th of October, 2022, to the 15th of April, 2023.
In Brazil, the WFPHA has built a strong and longstanding partnership, receiving substantial support from the Brazilian Association of Collective Health (ABRASCO). ABRASCO members and other health-related organizations were contacted through various official communication channels, such as newsletters, websites, and social media. To reduce non-response or selection bias,29 other national public health associations facilitated the survey distribution via email to their entire membership at various intervals, including the survey link in their newsletters and blogs, on their websites, and on social media. Regular reminders were sent to encourage participants to provide feedback. A STROBE statement is attached in Table S6.
2.2. Sample
This is an anonymous web-based cross-sectional study, adopting a non-probability sampling method to maximize the outreach of HCWs through a cost-effective approach.30 This method provides unique opportunities for population surveys,31 and is commonly adopted with the topic of COVID-19 vaccine intentions.16,18,32–34
2.3. Measures
2.3.1. Participants’ characteristics and VH
Participants’ characteristics include social demographics, knowledge of the COVID-19 vaccine, and fear of getting the virus. Socio-demographics included 7 questions (Q1, 2, 4-8 in questionnaire)28: gender, age, membership of the public health associations, highest level of education, profession, and primary work setting. Participants’ reports on chronic diseases indicated the presence or absence of pre-existing co-morbidity. Each of these was nominally recorded, except for age, which was divided into six categories for group comparison, aligning with a prior study.28 Knowledge of the COVID-19 vaccine (Q21) and fear of getting the virus (Q16) were assessed by two 10-point Likert scale questions with answers ranging from 1 (not at all) to 10 (very much). Based on the definition8 and prior results,28 questions about vaccine history (Q11, 13), vaccine uptake reasons (Q14), and vaccine intentions (Q15) were used to determine vaccine-hesitant or vaccine-non-hesitant (decision tree is presented in Figure S1).
2.3.2. Vaccine attitude and VH psychological constructs
Vaccine attitude was assessed by 17 questions: 6 for general vaccine attitudes (Q9-1 to 9-6) [e.g., Vaccines are scientifically tested and are among the safest pharmaceutical products?], and 11 for COVID-19 vaccine attitudes (Q10-1 to 10-11) [e.g., The risk of complications due to COVID-19 disease is greater than the risk of serious adverse effects from COVID-19 vaccine?]. Responses were rated on a 4-point Likert scale, ranging from 1 (strongly disagree) to 4 (strongly agree). Exploratory factor analysis (EFA) was performed on the above 17 attitude questions to explore the latent psychological constructs associated with VH, reflecting the 5C model in Brazilian HCWs.
2.3.3. Information sources and VS
The information sources data comes from Q20 [What sources do you consult to expand your knowledge of COVID-19 vaccines?]. 10 sub-questions included institutional websites (the Ministry of Health, the World Health Organization, or health authorities), publications from scientific societies, colleagues and other HCWs, social media (Facebook, Instagram, and Twitter), and etc. VS was determined by 5 sub-questions (of Q25) on vaccine attention (VS1), vaccine intention (VS2), vaccine confidence (VS3), general attitude (VS4), and health system confidence (VS5). Responses were dichotomized into “agree” (strongly agree, agree) and “disagree” (strongly disagree, disagree) categories.28
2.4. Statistical Analysis
Description analyses (RO1, RO2) were performed using IBM SPSS Statistics version 25.0 (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. IBM Corp, Armonk, NY, USA). The VH classification, EFA (RO3), and multivariate logistic regression (RO4, RO5) were performed by R software (R version 4.2.2). For RO3, Kaiser-Meyer-Olkin (KMO) and Bartlett’s test of sphericity were used to confirm data suitability for EFA. For RO4, multivariate logistic regressions were employed to associate explanatory variables, including 5 psychological constructs from RO3, with 5 VS. Missing data were ruled out for analysis; only completely answered respondents were considered in the inferential statistics. In multivariate logistic regression analysis, including RO4 and RO5, the multicollinearity between variables was checked by calculating the (generalized) variance inflation factors (VIFs). The significance level was set at 0.05. The estimated odds ratios (OR) and their 95% confidence interval (95% CI) were calculated and reported. We additionally reported McFadden’s pseudo R-squared, Hosmer-Lemeshow goodness-of-fit test, and the area under the receiver operating characteristic curve (AUC) to evaluate the explanatory power, model fit, and classification performance, respectively.
Results
3.1. Characteristics and VH (RO1)
Of the 634 participants (Table 2), 73.7% were female, and 23.6% were public health association members. The mean age was 46.0 (SD=13.7), and 49.2% were older than 44 years. For professions, 31.4% were nutritionists, 19.2% pharmacists, and 9.6% physicians, while 29.7% answered “other”. Regarding the highest level of education, 39.3% had a medical specialty/doctorate/postgraduate qualification; 23.2% had a bachelor’s degree; and 18.0% had a master’s degree. For primary work settings, 24.8% worked at university or research institutes, 15.9% in community services, 15.8% in private companies, 14.7% in hospitals (including hospice/long-term care, health centers, etc.), and 16.7% of respondents did not think their working setting fit with the listed categories. 24.3% suffer from chronic diseases, such as cardiovascular disease, diabetes, asthma, chronic obstructive pulmonary disease, cancer, HIV/AIDS, mental disorders, etc. The average self-reported knowledge scale was 7.3 (SD=1.7), suggesting most of the respondents were confident with their knowledge of the COVID-19 vaccine. The fear scale was 8.0 (SD=2.9), indicating that participants’ fears of contracting COVID-19 influenced their choice of receiving the COVID-19 vaccine. Only 25 (3.9%) were classified as vaccine-hesitant; therefore, further analysis for VH is limited.
3.2. Vaccine attitude and VS (RO2)
For vaccine attitudes (Table 3), 98% agreed that getting vaccinated is necessary, 95% were convinced about the safety, 86% believed in the vaccine effectiveness, and 81% thought that taking vaccines is in the community’s best interest. However, 50% believed that pharmaceutical companies downplayed the side effects of vaccines, 41% thought that public health authorities were doing the same. With regards to COVID-19 vaccination, 97% stated that easy access to the vaccination is crucial, 95% agreed with the vaccine effectiveness, 94% believed that the vaccine’s benefits outweigh the risks. 93% opined that children and adolescents should be vaccinated, 91% believed that community/religious/cultural leaders and traditional healers should reinforce the positive message about vaccination.
For VS, 84.4% will keep attention on vaccination (VS1), 82.5% expressed positive vaccine intention (VS2), 76.4% expressed enhanced vaccine confidence (VS3), 73.8% indicated their general attitude (VS4) has not been altered, and 71.7% reported an increased confidence in the health system (VS5) (Table S2).
3.3. VH psychological constructs (RO3)
Prior to EFA, seventeen vaccine-attitude questions were examined for completeness and suitability. The KMO measure was 0.94, and Bartlett’s test of sphericity was significant =6930.03, df=136, p<.001), indicating appropriateness for EFA. The EFA was performed using the maximum likelihood extraction method with oblimin oblique rotation, as several factors showed substantial intercorrelations (up to r = 0.80).
The optimal number of factors to retain was determined by a combination of statistical fit and theoretical justification. The scree plot with the parallel analysis is presented in Figure S2, suggesting retaining at most five factors due to their empirical eigenvalues exceeding the 95th percentile of the simulated eigenvalues. To identify the best solution, we evaluated the model fit indices across 3-, 4-, and 5-factor models. The 5-factor model emerged as the best-fitting one. It was supported by the smallest root mean square residual (RMSR = 0.02) and root mean square error of approximation (RMSEA = 0.044, 95% CI: 0.033-0.055), along with the highest Tucker-Lewis Index (TLI = 0.975). Although the 5-factor model had the second-lowest Bayesian Information Criterion (BIC), the difference compared to the 4-factor model was minimal.
The 4-factor model reflects 4 psychological constructs from the 5C model, except “calculation” (Table S1-1). The “constraints” show a negative correlation with the other 3 constructs (Table S1-2). The 5-factor model (Table 3) also includes 4 psychological constructs from the 5C model, which still hinder “calculation,” while considering factor loadings larger than 0.26 as significant. This exploratory approach implied that “collective responsibility” was constituted with 2 distinct constructs. Reflecting on the literature2,9 and our questions from the questionnaire, general collective responsibility (GCR) and obligated collective responsibility (OCR) were conceptualized and employed to further examinations. GCR was operationalized through items assessing measures toward the general public, such as adults, children, adolescents, or pregnant women. OCR was operationalized through items focusing on HCW-related measures. Each factor was assessed using Cronbach’s alpha (range 0.78–0.88).
The correlation between the 5 factors is presented in Table S3. The “complacency” is negatively correlated with the other 4 factors, with correlations ranging from -0.29 to -0.11, while the other 4 are moderately positively correlated with each other (r = 0.63-0.80). This indicates that higher levels of responsibility, confidence, and obligation are associated with lower complacency toward VH. Finally, the factor scores were estimated by the regression method and were used as determinants in logistic regression, subsequently.
3.4. Characteristics, psychological constructs, and VS (RO4)
Table S2 presents the odds ratios, 95% CIs, p-values, and overall model fit indices from the logistic regression analyses on the associations between VS and other explanatory variables, including characteristics and the five psychological constructs extracted from the previous EFA. In the VIFs assessment, four models (VS1, VS3, VS4, and VS5) showed potential multicollinearity issues, mainly because the VIFs for the GCR and OCR constructs in these models range from 5.4 to 7.8, while all other explanatory variables had VIFs well below the threshold of 5. This finding is not unexpected, as the EFA results (see Table S3) indicated a strong correlation (r = 0.80) between GCR and OCR, suggesting they are not entirely independent factors. However, to maintain theoretical integrity in this exploratory analysis, both constructs were retained in the models. It is worth noting that a supplementary analysis, presented in Table S1-1, explores a more parsimonious 4-factor solution where GCR and OCR are merged into a single “Collective Responsibility” construct. In this alternative specification, the multicollinearity issue is resolved across all logistic regression models.
Regarding model fit, the Hosmer-Lemeshow test indicates that, with the exception of the model for VS3, which showed a significant lack of fit (p = 0.026), all other models fit the data well, showing no significant discrepancy between observed and predicted outcomes. The model for VS2 (intention to receive a future COVID-19 vaccine) was particularly robust, demonstrating excellent explanatory power (McFadden’s R² = 0.523) and outstanding discrimination (AUC = 0.940). Although the model for VS3 failed the Hosmer-Lemeshow test, its McFadden’s R² (0.232) and AUC (0.798) values suggest it still possesses acceptable explanatory power and good discriminative ability. The models for VS1, VS4, and VS5 showed modest but acceptable performance in terms of their McFadden’s R² and AUC values.
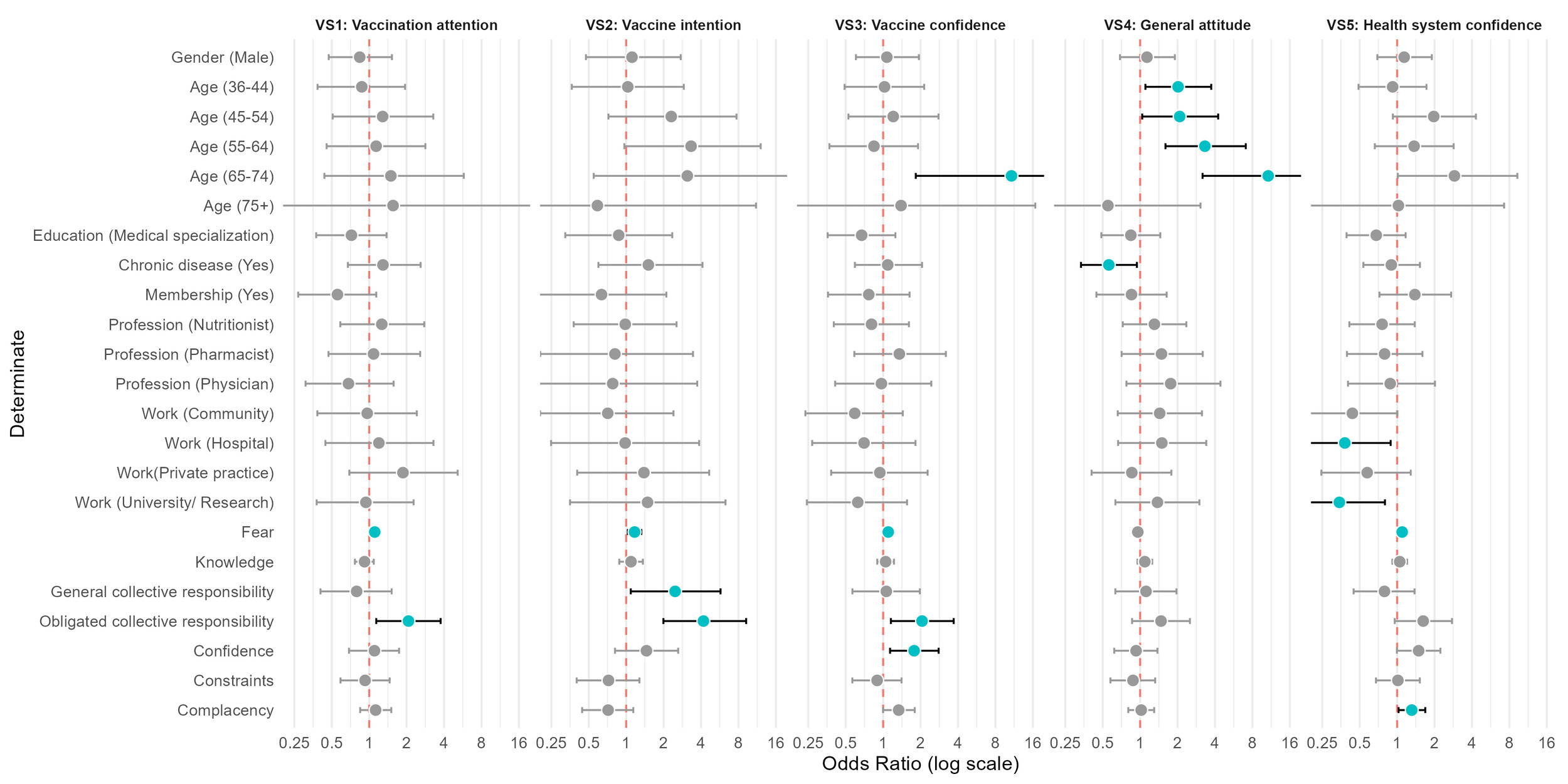
Figure 1 provides a forest plot of the odds ratios with 95% CI of each determinant. There is no significant difference in VS based on gender, education, membership status, or profession. Vaccine attention is positively associated with fear (OR = 1.11, 95% CI: 1.01-1.22) and OCR (OR = 2.07, 95% CI: 1.14-3.74), while vaccine intention is positively linked to fear (OR = 1.17, 95% CI: 1.03-1.32), GCR (OR = 2.47, 95% CI: 1.08-5.66), and OCR (OR = 4.18, 95% CI: 1.95-8.95). Vaccine confidence is notably higher among individuals aged 65-74 (OR = 10.77, 95% CI: 1.24-93.36) and is influenced by factors such as fear (OR = 1.1, 95% CI: 1.00-1.21), confidence construct (OR = 1.77, 95% CI: 1.13-2.78), and OCR (OR = 2.06, 95% CI: 1.15-3.66). General attitudes towards vaccination are more positive with increased age, but lower with those with chronic diseases (OR = 0.56, 95% CI: 0.33-0.94). HCWs working in hospitals (OR = 0.38, 95% CI: 0.16-0.90), university or research settings (OR = 0.34, 95% CI: 0.14-0.82) showed lower confidence in the health system while both fear (OR = 1.10, 95% CI: 1.01-1.19) and complacency (OR = 1.31, 95% CI: 1.03-1.68) play a role in shaping this confidence.
Supplementary analysis was conducted to associate VS, fear, and psychological constructs, considering the results between the 4-factor (Table S4-1) and 5-factor (Table S4-2) solutions. In the 4-factor solution, collective responsibility is positively related to vaccine confidence (OR = 2.12, 95% CI: 1.34-3.36) and vaccine intention (OR = 8.39, 95% CI: 4.15-16.97). However, in the 5-factor solution, GCR is not associated with any VS. OCR is positively related to vaccine attention (OR = 1.96, 95% CI: 1.13-3.40), confidence (OR = 2.08, 95% CI: 1.22-3.53), and intention (OR = 3.70, 95% CI: 1.90-7.18). This possibly implies the importance of OCR rather than GCR in our case.
3.5. Information source and VS (RO5)
Regarding information sources and VS, Table S5 presents the odds ratios, 95% CIs, p-values, and overall model fit indices from the logistic regression analyses for each VS. All VIFs of the information sources are smaller than 1.55, indicating there is no multicollinear problem in the data.
In addition, all models do not demonstrate a lack of fit, with p-values of the Hosmer-Lemeshow test all exceeding 0.05. Nevertheless, the models exhibited limited explanatory power and discriminatory ability, as indicated by low McFadden’s R² values (0.019–0.089) and low AUC values (0.596–0.689). Of the five, VS2 performed relatively best, with a McFadden’s R² of 0.089 and an AUC of 0.689.
Figure 2 provides a forest plot of the odds ratios with 95% CI of each information source. Institutional websites were the major source for information (85.4%), followed by scientific societies’ publications (70.8%), colleagues and other HCWs (55.3%), and scientific organizations’ webinars or courses (54.1%). Community members (3.6%), friends and family (6.5%) were less common.
Institutional websites from health authorities (e.g., World Health Organization or Ministry of Health) play a significant role in shaping vaccine intention, vaccine confidence, and health system confidence. Scientific societies were negatively linked to health system confidence (OR = 0.59, 95% CI: 0.36-0.97). Information from other websites significantly hindered HCWs’ vaccine intentions (OR = 0.41, 95% CI: 0.20-0.86).
Discussion
Table 1 summarizes key results for each secondary RO. The prevalence of VH was low among participants (n=25), limiting the statistical power to analyze its determinants robustly. Nonetheless, VH appeared more prevalent among HCWs aged over 35, consistent with prior studies suggesting age-related differences in vaccine perceptions35,36 and possibly reflecting generational differences in risk perception, vaccine experience, and information preferences.16,33,37 While participants reported high trust in vaccines themselves, they also expressed persistent skepticism toward institutions, pharmaceutical companies, and media sources, which aligns with previous research.2,17,20,21,35,38,39
This institutional skepticism is situated within a recent national context where the federal government’s promotion of unproven treatments and resistance to mass vaccination diminished public trust, impacted HCW self-efficacy,39 and contributed to Brazil becoming a major reservoir for SARS-CoV-2 variants.40 This political climate has reportedly begun to reverse under the current administration, which has renewed its commitment to scientific guidance and vaccination campaigns.41
Our findings support the 5C model’s utility for understanding HCW vaccine attitudes and, more importantly, propose a key conceptual refinement: distinguishing “Collective Responsibility” into two distinct forms: GCR, a voluntary moral drive, and OCR, a professional duty inherent to an HCW’s role,2,9–13,15,42 However, “calculation” doesn’t reflect from the data, possibly due to our questionnaire design. GCR was operationalized through items assessing measures toward the general public, such as adults, children, adolescents, or pregnant women. OCR was operationalized through items focusing on HCW-related measures. This distinction is particularly important for HCWs because their motivation to vaccinate is shaped by professional factors beyond those that influence the general public, including high confidence in their clinical knowledge1 and acute awareness of infection risks.2 This theoretical refinement was borne out by our data.
While the broad “Collective Responsibility” construct correlated with vaccine intention and confidence (Table S4-1), our refined model revealed a crucial divergence: OCR was significantly associated with vaccine intention, confidence, and attention, whereas GCR was linked only to vaccine intention (Table S4-2). The strong association between the OCR construct and positive vaccination outcomes suggests that policies appealing to professional duty, such as vaccine mandates or workplace protocols, may be a promising avenue for improving vaccine acceptance.
Furthermore, our analysis indicates that distinct determinants are linked to specific facets of VS, suggesting that a one-size-fits-all approach to intervention is likely insufficient. For example, a more positive general attitude toward vaccination was associated only with demographic factors (older age, no chronic disease), not the psychological constructs we measured. This implies that interventions aiming to improve general attitudes might focus specifically on younger HCWs or those with chronic conditions. In contrast, lower confidence in the health system was reported by HCWs in hospital, university, or research settings, perhaps reflecting the heightened institutional skepticism documented in prior studies.20,21 This finding highlights a potential need for targeted, trust-building initiatives within these specific environments.
Our findings also highlight the critical role of institutional websites as a trusted channel for disseminating information to HCWs. HCWs showed a clear preference and trust for sourcing information from institutional websites and publications from scientific societies41 over more time-intensive formats like webinars or courses, a choice likely driven by demanding professional schedules. This preference for easily digestible or less time-consuming information20 may also explain why the “Calculation” component of the 5C model did not emerge as a significant factor in our analysis. Notably, while prior work has underscored the influence of religious affiliation43 and social media,44,45 our findings suggest neither was a primary information source for this HCW cohort. However, neither is the main information source for Brazilian HCW. Therefore, a key recommendation from this study is that public health campaigns should partner with these trusted institutional bodies to deliver clear, concise, and easily accessible information to HCWs, particularly during future health crises.21,46,47
Nevertheless, it’s essential to acknowledge some limitations. First, our reliance on convenience sampling through an anonymous online questionnaire introduces a significant potential for selection bias. While this method was intended to maximize participation and encourage candid responses, it means our findings cannot be considered representative of the broader Brazilian HCW population. Besides, this encourages non-ABRASCO and diverse socio-demographic HCWs to participate in this project, which extends the scope of this study.
Second, the study’s interpretation is limited by a potential cultural misalignment, as the survey instrument was designed for a multinational project and did not fully map onto the Brazilian context. For example, the question on the “highest level of education” may have been confusing, as some professional health specialties in Brazil are not classified as formal academic degrees in the same way they might be elsewhere. This misalignment is the likely cause of the high frequency of “Other” responses for questions on profession and education, which in turn complicates interpretation and increases the risk of misclassification bias.28 To mitigate this issue in the future, cross-cultural surveys should incorporate culturally-adapted examples within response options, preventing respondents from being forced into a generic “Other” category.
Third, key statistical limitations affect the certainty and generalizability of our findings. As an exploratory study, our analysis did not adjust for multiple comparisons. While this approach increases the potential for Type I errors (false positives), it was chosen intentionally to prioritize sensitivity and avoid prematurely dismissing associations that may warrant future investigation. Consequently, the specific associations identified here should be interpreted as preliminary hypotheses requiring confirmation in future, larger-scale studies. Furthermore, the findings are specific to HCWs and may not be generalizable to the general public, given HCWs’ distinct levels of clinical knowledge.2
Fourth, the study’s cross-sectional design precludes any conclusions about causality. While our analysis identifies significant associations, it cannot determine the direction of these relationships. For example, it is unclear whether higher trust in institutions leads to vaccine acceptance or if the act of getting vaccinated and having a positive experience subsequently builds trust. Therefore, longitudinal and experimental studies are needed to untangle these potential causal pathways and validate our findings.
CONCLUSIONS
This study identified determinants of vaccine sentiment (VS) in a cohort of Brazilian HCWs and proposed a theoretical expansion of the 5C model to better capture this group’s unique motivations. To our knowledge, this is the first empirical study to differentiate General Collective Responsibility (GCR) from Obligated Collective Responsibility (OCR) within the 5C model, a crucial distinction that reflects the dual roles of HCWs as both private citizens and public health advocates. A conceptual framework is presented to illustrate the relationship between characteristics, 5 psychological constructs, information sources, and VS among Brazilian HCWs (Figure 3). Our findings suggest that enhancing VS among HCWs requires a two-pronged approach: 1) ensuring access to accurate information through trusted institutional channels, and 2) leveraging their sense of professional duty (OCR) through supportive, ethics-based workplace policies. Future research should build on these findings by employing culturally-adapted instruments, qualitative methods to deepen understanding, and longitudinal designs to investigate causality. We particularly recommend that large-scale quantitative studies include a qualitative component to capture the vital local contexts that numbers alone cannot.
Acknowledgements
We would like to acknowledge all health-related organizations in Brazil who have supported the WFPHA study by sharing the survey within their network, as well as the members of the WFPHA International Immunization Policy Taskforce for their valuable input. Additionally, we would like to thank Andrea Parisi, who gave valuable insights into this study.
Ethics statement
This research, conducted by the WFPHA, headquartered in Geneva, complied with Swiss legislation regarding ethics approval, particularly the Federal Act on Research involving Human Beings. The study was exempted from review by the Geneva Cantonal Research Ethics Commission (Req-2022-00421). It adhered to Good Clinical Practice (GCP) and Good Epidemiological Practice (GEP) standards, as well as the Declaration of Helsinki and EU Regulation No 2016/679 (GDPR) about data processing.
Funding
The WFPHA has received an unrestricted grant from GSK for a broad project on vaccine hesitancy. The funders had no role in the study’s design, in the collection, analyses, or interpretation of data, in the writing of the manuscript, or in the decision to publish the results. GSK Biologicals SA was invited to review a preliminary version of the manuscript for factual accuracy. Authors are solely responsible for the content and interpretation, minimizing the potential bias from the involvement of industry funding.
Authorship contributions
C. L. and TY. L. conceived of the presented idea, developed the structure, performed the computations, and wrote the manuscript with input and discussion from all authors. L. R. conducted the primary data analysis. M. M and M. L. applied for funding. All authors discussed the results and contributed to the final manuscript
Disclosure of interest
Michael Moore has received honoraria and travel support from Pfizer and MSD.
Correspondence to:
Name Surname: Chungwan Lo
Institution: World Federation of Public Health Associations; Department of Prevention and Evaluation, Leibniz Institute for Prevention Research and Epidemiology – BIPS
Address: Achterstraße 30, 28359 Bremen
Country: Germany
lo@leibniz-bips.de
Name Surname: Marta Lomazzi
Institution: World Federation of Public Health Associations; University of Geneva
Address: Institute of Global Health, University of Geneva, Campus Biotech - G6, chemin des Mines 9, 1202 Geneva, Switzerland
Country: Switzerland
marta.lomazzi@wfpha.org