A well-trained public health workforce is critical for global health security to prevent, detect, and respond to public health emergencies (e.g., epidemics, man-made disasters) anywhere in the world.1–6 E-learning or online training delivered asynchronously (i.e., self-paced learning with recorded materials) and/or synchronously (i.e., real-time learning through video conferencing) is a rapidly evolving training delivery method that is driven by advancements in information and communication technology (ICT). Unlike face-to-face (F2F) method, e-learning is not bound by physical interaction, geographic location, and time requirements, thus offering greater flexibility for the delivery of training instructions as demonstrated, for example, during the COVID-19 pandemic, where in-person activities were restricted.7–11 Though, e-learning has some limitations, ranging from low interactivity to delayed receipt of instructor feedback, as well as high learning tasks (e.g., concurrent listening and navigation of ICT tools), its flexibility and relative advantages (e.g., high reach and cost effectiveness) have been attributed to the paradigm shift from F2F training to novel e-learning interventions among public health workers globally, including those in Africa.7–16 More so, evidence shows that e-learning is associated with improved learning outcomes as demonstrated in several meta-analysis, where they reported improvement in knowledge of health professionals exposed to e-learning compared to those with F2F method.8,17–19 To maximize learning outcomes, a multi-communication online training (MOT), which is described as an e-learning intervention that incorporates a combination of synchronous and asynchronous online methods with a wide range of ICT-enabled approaches (e.g., facilitated learning, and social media-based learning) has been identified as a promising practice for e-learning.12,20
Similar to other regions of the world, there has been some progress in the implementation of e-learning among the public health workforce in Africa, which has grown from an era of university-led online trainings to public health institutions-led trainings such as the World Health Organization’s Integrated Disease Surveillance and Response (WHO IDSR) and the Africa Centres for Disease Control and Prevention Institute for Workforce Development (CDC IWD)'s leadership and management online courses.21–23 However, the contextual fit and feasibility of any of these e-learning interventions remain poorly understood. More so, while the adoption of e-learning interventions continues to increase in Africa, which is in part accelerated by the COVID-19 pandemic, its implementation in the public health sector remains fragmented, uncoordinated, and inequitable due to numerous problems, including digital divide, economic inequality, and other system-level factors (e.g., lack of workplace ICT policies, and unstable electric power).7,8,11,24–26 Thus, limiting the potential of maximizing their benefits for capacity building of the public health workforce in performing its core functions. This is especially important because the African continent shares as high as 39.2% of the global burden of epidemic- and pandemic-prone diseases that are managed by its public health workers, who account for only 3% of the global health workforce.5,6,27 Hence, indicating a critical shortage of the expertise needed to address the public health needs of the communities in the continent. Further, the West African subregion suffers a disproportionate impact from these problems, where it accounts for 36.4% of the epidemic- and pandemic-prone diseases burden, as well as 41% of the health workforce shortage in the African region.6,28 Given this body of knowledge, understanding the “degree of influence” of these problems in their trainings through contextual fit and feasibility assessments, as well as the “how of influence” that is established by associated factors becomes very important for implementation of e-learning to inform its adaptation and scale up towards improving accessibility and usability of essential health information among public health workers for public health emergency management.
In addition, the translation of the definitions of contextual fit (i.e., “how well the program or practice aligns with the implementing site and focus populations’ perceptions of strengths and needs, values, culture, and history, other initiatives and priorities, as well as internal capacity resources available for implementation”) and feasibility (i.e., “how well the program or practice can be integrated into the implementing site based on how operationalized the program or practice is, the supports available at the site to support implementation, and the strength and availability of research data”),26 into practical information suggests that the usual assessment of contextual fit and feasibility of evidence-based interventions (EBIs) like e-learning with a single construct of preference or acceptability, or willingness to use in either case of contextual fit and feasibility due to the lack of a consensus in their assessments, may not give the true estimates of these implementation outcomes in a real-world situation. Also, the interpretation of the ratings of contextual fit and feasibility (i.e., high, or low) by any of these constructs is subjective due to the lack of empirical thresholds.29,30
Although, findings from a few studies provided some insights into the contextual fit and feasibility of e-learning among the public health workforce in Africa, including a meta-analysis conducted between 2020 and 2022 that showed an e-learning willingness to use rate of 49.5%, and a preference rate of 29.7% that is marginally comparable to F2F (33.5%),12 as well as an acceptability rate of 90.5% reported in another study.16 The rating of these constructs is challenging and their generalizability is limited in making meaningful conclusions because of lack of a representative sample population by country (i.e., studies are usually conducted in a single country) or work setting (i.e., studies are predominantly hospital-based and exclude other settings such as community-based organizations), or work sector (i.e., studies are mostly human health-focused and exclude other sectors such as animal health), including a scarcity of qualitative evidence.8,17–19 More so, while there is an overwhelming evidence on the downstream factors (e.g., sex, age) that are associated with acceptability of and willingness to use e-learning interventions, there is a gap in knowledge about how upstream factors (e.g., workplace ICT availability, financial incentives) and midstream factors (e.g., self-efficacy, performance expectancy) mediate the acceptance and use of e-learning among the public health workforce in most settings, including Africa.7,8,26 To support effective implementation and scale up of e-learning interventions for global health security, we conducted a mixed-methods study using a novel pragmatic rating tool to assess:
-
The contextual fit of MOT (with outcomes on preference and acceptability) and associated factors; and
-
The feasibility of MOT (with outcomes on willingness to use and workplace ICT availability) and associated factors among public health workers in 16 West African countries.
METHODS
This is a cross-sectional study with mixed-methods concurrent design that involved a quantitative survey and qualitative interviews. Online survey and in-depth interviews (IDIs) were used to determine the views of public health workers on the constructs, including preference; acceptability; willingness to use; and workplace ICT availability towards MOT to inform understanding of its feasibility and contextual fit in West Africa. The qualitative data provided more information on how and to what extent these objectives were perceived by public health workers, including practitioners, managers, trainers, and policymakers. Quantitative data were triangulated with qualitative data to explain the contextual fit and feasibility of a MOT intervention in the subregion. The study was conducted from Aug 10, 2023, to Oct 10, 2023. Throughout this study, we followed the Good Reporting of a Mixed-Methods Study (GRAMMS) checklist (Appendix 1),31 in addition to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline. This study was approved by the Emory University Institutional Review Board and the West African Health Organization (WAHO). All participants provided informed consent prior to the quantitative survey and qualitative interviews, as well as the permission to have the interviews audio-recorded.
Study settings
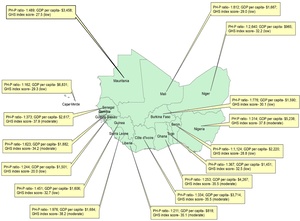
To improve representativeness, all 16 countries of West Africa were included in this study. The countries were stratified by the three main official languages in the subregion: English (The Gambia, Ghana, Guinea, Liberia, Nigeria, Sierra Leone); French (Benin, Burkina Faso, Cote d’Ivoire, Mali, Mauritania, Niger, Senegal, Togo); and Portuguese (Cape Verde or Cabo Verde, Guinea-Bissau). These countries differ by public health worker-population (PH-P) ratio, economy, and emergency preparedness and response (EPR) capacity (Figure 1). The subregion is reported to have a total of 1,054,042 public health workers serving a population of 390,953,045 (i.e., PH-P ratio of 1:371), an average gross domestic product per capita of $2,594, and an average global health security index score of 32.3 of a possible score of 100 prior to the COVID-19 pandemic.32–35
Study participants and sampling
Using the One Health approach, public health workers across the human, animal, and environmental health sectors in West Africa were invited to voluntarily participate in quantitative survey and qualitative interviews. Participants in this study included public health workers in three groups based on the WHO EPR action plan,3 including core public health workers (public health specialists); healthcare workers with one or more public health functions (physicians, nurses, laboratory scientists and technicians); and allied workers (environmental health scientists and technicians, veterinarians and assistant veterinarians). The estimated sample size for the quantitative survey was 222 based on an expected proportion of 90.5% of public health workers that considered e-learning as an acceptable modality of training in an African setting at 95% confidence, and after adjusting for a non-response rate of 40% for most online surveys focused on e-learning topic.16,36
n= Z2 P(1−P)d2
Z (standard deviate at 95% confidence): 1.96
P (estimate of true proportion):0.905
d (level of significance):0.05
= 1.962 × 0.905 (1−0.905)0.052
= 1.96 × 1.96 × 0.905 × 0.0950.05 × 0.05
= 0.330281560.0025 =133
Adjusting for non-response rate of 40%,
= 1331−non response rate = 1331−0.4 =222
A total of 231 public health workers completed the survey. Of the total survey responses, 146 (63.2%) were completed in English, 80 (34.6%) in French, and 5 (2.2%) in Portuguese. For qualitative interviews, nine IDIs were considered sufficient to generate all relevant themes.37 However, we were only able to interview seven participants (four English and three French speakers) due to lack of Portuguese speaking proficiency among the research team. Participants were sampled for the quantitative survey using a virtual snowball technique. We identified 43 EPR focal persons across the human, animal, and environmental sectors in each study site from the West African Health Organization (WAHO)'s workforce database; they were then contacted via email to sensitize them about the study. Second, a follow-up email was sent to: (1) complete the study’s pre-test survey via Google Forms; and (2) participate in an online forum via Zoom, where they received more information about the study’s objectives and were requested to assist in wider dissemination of the main survey’s Google Forms to their colleagues and networks using any communication media (e.g., email, social media).
For the qualitative interviews, we recruited interviewees from the EPR focal persons that participated in the online forum using voluntary response sampling technique given that the study population were appropriately represented in the forum sample. Of the 27 participants that attended the online forum, we had 12 diverse participants from the human, animal, and environmental health sectors that expressed interest in the IDIs, out of which seven confirmed their availability and were included in the IDIs.
Framework and instruments
Quantitative data were collected using a self-designed, semi-structured questionnaire. The development of the survey questionnaire was guided by our newly proposed pragmatic contextual fit and feasibility (PCoF) tool framework and scoring or rating system designed with theoretical underpinnings from knowledge-to-action framework and a modified unified theory of acceptance and use of technology,38,39 which depicts how outcomes of preference and acceptability of EBI could interact to inform contextual fit, as well as how interactions of willingness to use an EBI and resource availability outcomes inform feasibility (Appendix 2, 3). The survey contained a total of 23 questions that correspond to ten categories: sociodemographic information (job discipline, age, sex, years of experience, work setting, work sector, work area, work country); personal ICT accessibility; previous e-learning; workplace internet funding; ICT acceptability and use mediating factors (self-efficacy, effort expectancy, performance expectancy, attitude, social influence); contextual fit (MOT acceptability, MOT preference); feasibility (MOT use willingness, workplace ICT availability), including questions on perceived ICT constraints and enablers, and recommendations for e-learning delivery that are reported in another study. Additionally, we used “e-learning preference” as a proxy measure of “MOT preference” with the assumption that those who prefer to be trained via e-learning are likely to prefer any approach (e.g., multi-communication) used in its delivery. The survey questions were mostly closed-ended with a few that were open-ended. The open-ended questions included parts of the survey where participants could enter their responses for “other” answer option, and the question on recommendations for e-learning delivery. To reduce response bias from guessing, “Not sure” was included as part of the answer options where appropriate. The survey questionnaire was created in English and translated into two languages: French, and Portuguese, and back translated to English by the translation unit of WAHO to ensure that meaning was retained (Appendix 4). Quantitative data were collected online using Google Form (Google LLC, Mountain View, CA, USA) with a user-friendly interface. The survey Google Form link was created for each language.
The qualitative interviews were guided by the PCoF framework constructs (acceptability, preference, willingness to use, resource availability). Guided by this framework and in line with the quantitative survey, our IDIs guide focused on interviewees’ opinions on how they perceive preference; acceptability; willingness to use; and workplace ICT availability towards implementation of MOT, and the underlying reasons for their perceptions (Appendix 5).
Data collection
The survey questionnaire was pilot tested among 39 public health workers, who represented a majority of study sites. The average completion time for the survey was about 10 minutes. Recipients of the pilot-test survey had no suggestions for improvement of the questionnaire. To reduce missing data and low response associated with online surveys, responses to all questions were made “required” for the survey to be successfully completed. The survey link was shared via email to focal public health personnel in each study site identified from the workforce database of WAHO. These focal persons were encouraged to further share the survey link among their subregional public health networks to achieve a virtual snowball sampling. Only focal persons who did not complete the pilot-test survey were required to complete the main survey before sharing the link with their networks. Responses from the pilot-test survey were not included in the final analysis. To increase participation of the target population, the survey was also promoted through the WAHO website, newsletter, and social media. The Africa Centers for Disease Control and Prevention (CDC) and the African Field Epidemiology Training Network (AFENET) were contacted to promote subregional participation. Responses to the survey questionnaire were voluntary and anonymous. All were asked to give informed consent in the online survey before being prompted to respond to the questions and were informed that they could withdraw at any time of the survey. To protect privacy of the participants, no personally identifiable information (e.g., email) of the participants were recorded in the Google Forms during completion of the survey. Confidentiality was ensured by not sharing the data to anyone outside of the research team. The survey responses were automatically generated into an Excel spreadsheet by the Google Form’s software and combined.
The qualitative interviews were conducted among public health experts (e.g., managers, trainers, policymakers) with varying experience across the human, animal, and environmental health sectors. A semi-structured IDIs guide was developed with nine open-ended main questions with associated seven probing questions. A broad data-generating question was first used: “tell me about your work experience”. Open-ended main questions were used to obtain detailed descriptions (e.g., “can you describe a particular training modality that is mostly used in your workplace”; and “what are your thoughts on the acceptability of a multi-communication, online training among practitioners in your field”). Probing questions ranged from non-specific questions (e.g., “Please tell me more about that”) to specific questions (e.g., “could you describe what you think are some of the factors that may influence the acceptance of a multi-communication, online training among practitioners in your field”). The IDIs guide was created in English and translated to French. Consistent with the quantitative survey, our IDIs guide focused on interviewees’ opinions on how they perceive preference; acceptability; willingness to use; and workplace ICT availability towards implementation of MOT, and the underlying reasons for their perceptions. The IDIs also explored their thoughts on existing ICT constraints and enablers, including their recommendations for e-learning delivery that are reported in a study elsewhere (Appendix 5). The IDIs guides were not pilot-tested due to a small sample of available participants that volunteered to be interviewed. The IDIs were facilitated by two members of the research team (KOO and LSS), who have English and French speaking proficiency respectively and are experienced qualitative interviewers. The IDIs were conducted via an institutional-sponsored Zoom platform (Zoom Video Communications Inc, CA, USA) in a private and quiet location. The main and probing questions were added or removed through the course of the IDI depending on the type of responses provided. Examples of instances that necessitated these modifications include the interviewee bringing up an issue that required clearer explanation, an interviewee answering a question in a closed manner, or an interviewee having already thoroughly described an issue in a previous part of the IDIs. We conducted the IDIs until thematic saturation was reached for each interviewee and no new themes were emerging. The IDIs took approximately one hour. With interviewees’ permission, the IDIs were concurrently audio-recorded and transcribed verbatim during each session using the Zoom’s in-built recording and multi-language transcript services. The IDIs were transcribed verbatim in English and French languages respectively. By listening to the audio recordings in multiple sequences, all verbatim transcripts were reviewed by the interviewers for accuracy. The verbatim transcripts in French were translated to English. The IDIs were voluntary, and all interviewees were asked to give verbal informed consent before each interview and were informed that they could withdraw at any time of the interview without any penalty or loss of benefits to which they may be otherwise entitled. All transcripts were de-identified to ensure confidentiality. All personally identifiable information was removed from the transcripts, for example, by replacing names with generic phrases and numbers (e.g., public health specialist PH1, veterinarian V1). The audio recordings, and transcripts were stored on a password-protected computer prior to data analysis.
Data analysis
Quantitative data were cleaned and analysed using SAS version 9.4 (SAS Institute, Cary, North Carolina, USA). The study outcomes’ construct variables are MOT preference rate (defined as the proportion of participants who indicated e-learning as their preferrable training method); MOT acceptability rate (proportion of participants who found MOT as an acceptable method for their training); MOT willingness to use rate (proportion of participants who have the intention to use MOT for their capacity building); and workplace ICT availability rate (proportion of participants who reported accessibility to both computer and internet in their workplaces). Preference variable was created by coding “E-learning” answer to question 12 as “Yes”, and “Physical” and “Hybrid” answers as “No”. Workplace ICT availability variable was created by coding “Computer and Internet” answer to question 11 as “Yes”, and “Computer” and “None” answers as “No”. Since binary variables (i.e., variables which can have only a Yes or No value) are used in SAS statistical analysis of categorical outcome variables, “Not sure” and “No” responses were combined as “No” value as consistent with the study’s underlying assumptions (Appendix 2, 6). To improve representativeness in the results, statistical weighting procedure was employed with inverse probability weights and post-stratification weights at the country level using data from the World Health Organization (WHO) report on health workforce in the African region in 2018 to account for unequal probability of selection of participants, and due to differences in the distribution of baseline characteristic at the country level between our study sample and target population (Appendix 7, 8). The SAS survey procedure was used to account for clustering at the country level, and statistical weights. Unweighted frequencies, weighted frequencies, and weighted proportions of the categorical outcome variables were reported overall, and by country. Normality of numeric variables (age, experience) was assessed using Sharpiro-Wilk test given that our sample size is less than 2000, with variables determined as normal if p>0.05, and they were both found to have non-normal distributions. Normality was also assessed graphically using histogram (Appendix 9). Weighted medians and interquartile ranges (IQRs) were reported for age, and years of experience given their non-normality. Differences between distribution of independent variables or factors (job discipline, age categories, sex, years of experience categories, work setting, work sector, work area, work country, personal ICT accessibility, previous e-learning, self-efficacy, effort expectancy, performance expectancy, attitude, social influence, and workplace internet funds) associated with outcome variables were assessed using Rao-Scott Chi-square test and Fisher’s exact test. The factors that were significant at p<0.05 in the Rao-Scott Chi-square and Fisher’s exact tests were included in the bivariate analysis with binary logit regression model to evaluate factors that predicted the outcome variables. Associations between factors and primary outcome variables were assessed using multivariate binary logit regression models with traditional Maximum Likelihood estimates. Multicollinearity diagnostics were conducted to ensure that the independent variables included in the multivariate logistic regression models were not highly correlated with each other. Multicollinearity was established if two or more independent variables had eigenvalues close to 0, and variance decomposition proportions greater than 0.3 with corresponding condition index of 10-30 or higher, for which they were dropped in the multivariate logistic regression model. In analytical situations where quasi-complete separations (i.e., situations linear combinations of all or some of the independent variables yields a perfect prediction of the primary outcome variables that leads to non-convergence of and biased traditional Maximum Likelihood estimates) were detected in part due to our study small sample size, in addition to the inclusion of multiple independent variables, the Firth’s Penalized Likelihood regression technique was used to produce odds ratio estimates to reduce such analytical bias. And, in instances where complete separation persisted with a particular independent variable after the Firth’s Penalized Likelihood regression technique, the variable was excluded in the multivariate regression model. 3-level categorical variables (low, moderate, and high) were created to rank MOT preference; MOT acceptability; MOT willingness to use; and workplace ICT availability rates for easier interpretation. This was determined by geospatially calculated tertile cut-point values for each outcome variable rate at the country level using quantile data classification method in ArcGIS version 10.3.1 (Esri, Redland, CA, USA) because it is considered most appropriate for ordinal data, and their proportion distributions are presented with choropleth maps created by symbology procedure. For MOT preference, ranking was determined as “low” when the rate is ≤ 22.2%, “moderate” (22.3%-37.5%), and “high” (37.6%-100%), while MOT acceptability is ranked as “low” when rate is ≤ 87.5%, “moderate” (87.6%-95.0%), and “high” (95.1%-100%). For MOT willingness to use, ranking was defined as “low” when the rate is ≤ 92.3%, “moderate” (92.4%-95.0%), and “high” (95.1%-100%), while workplace ICT availability was ranked as “low” when rate is ≤ 37.5%, “moderate” (37.6%-72.7%), and “high” (72.8%-100%). A two-sided p<0.05 was considered statistically significant for all analyses.
Qualitative data were analysed using thematic analysis. The IDI transcripts were independently coded by 2 coders (the interviewers: KOO and LSS). The analysis included reading of the transcripts several times to gain understanding of the meanings conveyed and identify key issues. The key issues identified were used to create codes. A codebook was developed with code definitions, inclusion criteria, exclusion criteria, and examples. Coding was performed until thematic saturation was reached. Codes were then compared and discussed by the team until consensus on the themes was achieved. Thick descriptions were produced, and sufficient quotations collected from the transcripts for the themes to explain the research questions. Qualitative data were managed using Microsoft Excel and MAXQDA 10. Our qualitative data analysis was consistent with Braun & Clarke 15-point Thematic Analysis checklist (Appendix 10).40
Findings from the quantitative data and qualitative interviews were triangulated to understand preference, acceptability, willingness to use, and workplace ICT availability towards MOT among public health workers in West Africa using a joint display (Figure 2). The joint display was developed with meta-inferences that evaluated the coherence of the quantitative and qualitative findings by (1) “confirmation” (i.e., agreement between quantitative and qualitative findings); (2) “expansion” (i.e., existence of different aspects of the same phenomenon identified by quantitative and qualitative findings); and (3) “discordance” (i.e., disagreement between quantitative and qualitative findings).41 We used the PCoF tool’s 3-category qualitative ranking (strong, somewhat, weak) to explain contextual fit and feasibility. We presented the geospatial distribution of contextual fit and feasibility rankings at the country level using manual interval data classification method in ArcGIS by converting their 3-level categorical variables to percentages where “strong” was assigned a maximum score value of 3 (100%), “somewhat” a value of 2 (66.67%), and “weak” a minimum value of 1 (33%) to show the quantity of the variables relative to other score values (Appendix 3).
RESULTS
Sociodemographics
A total of 231 public health workers from 16 West African countries completed the quantitative survey for this study, with results computed for a population estimate of 2,873,004 after statistical weighting by country (Table 1). For the quantitative findings, we found that the median age of public health workers that participated in the survey was 39 (IQR= 34-46) years, while the median work experience was 10 (IQR= 6-16) years. Public health workers from urban areas accounted for a majority (78.7%) of the survey participants compared to those from rural areas (21.3%). The proportion of public health workers that participated who are males (63.5%) was higher than those who are females (36.5%). A greater proportion of public health workers in human sector (66.59%) participated than those in animal (18.85%) and environment (14.56%) sectors.
For qualitative interviews, a total of seven individuals were included for IDIs. The individuals interviewed were managers, trainers, and policymakers in their respective fields of public health. All were from urban areas with 4 females and 3 males. The IDIs included public health experts from human (n= 3), animal (n= 3), and environment (n= 1) sectors (Table 1).
Rate, associations, themes, and meta-inferences
MOT preference
Quantitative
Of the 231 public health workers, a population estimate of 29.61% (95% CI= 23.96-35.27) reported having preference for MOT. The MOT preference rate varied significantly by country (p= 0.0006), from the highest in Mauritania (87.50%) to the lowest in Cote d’Ivoire (7.69%) [Appendix 11 Table 1 and Fig. 1]. Quantitative findings showed that work area, age, sex, performance expectancy, attitude, previous e-learning, and workplace internet funding had statistically significant associations with MOT preference in both bivariate and multivariate analysis. MOT preference was less likely among public health workers in rural areas than those in urban areas (aOR= 0.58; 95% CI= 0.58-0.59). MOT preference was more likely among public health workers aged ≤ 29 years (versus 30-39 years, aOR= 58.22; 95% CI= 56.97-59.49) and 50-59 years (versus 30-39 years, aOR= 1.75; 95% CI= 1.74-1.76), and less likely among 40-49 years (versus 30-39 years, aOR= 0.40; 95% CI= 0.39-0.40). Female public health workers were more likely to have preference for MOT than those who are males (aOR= 2.54; 95% CI= 2.53-2.56). MOT preference was less likely among public health workers who reported lack of performance expectancy for MOT than those who had this attribute (aOR= 0.04; 95% CI= 0.03-0.04). MOT preference was less likely among public health workers who reported lack of internet funding in their workplaces than those who reported existence of workplace internet funding (aOR= 0.37; 95% CI= 0.36-0.37) [Table 2].
Overall, opinions from the public health workers that participated in the IDIs suggested a moderate preference for MOT, where three interviewees (42.86%) of a total of seven reported that public health workers are likely to prefer eLearning compared to three endorsements (42.86%) for F2F and one (14.28%) for hybrid, which was in discordance with the result from the survey. IDIs were analysed into training resources accessibility, training characteristics, and training environment themes with their respective meta-inferences (Table 2).
Qualitative
Training resources accessibility
Consistent with the survey findings, IDIs with the public health workers highlighted that access to ICT (computer, internet), which is mostly dependent on the work area (rural or urban) of a public health worker was one of the training resources accessibility factors that could influence the preference for MOT.
“So, the first thing is the cost attached. That is, the data or the internet, that is personally paid for that’s one that might discourage one from using that. Two is the equipment also, you need to have a computer and have a laptop. You also need to have a power source. So, it’s something that also might discourage someone from using it even when they have an opportunity to do it. Third, and also has to do with the person knowledge on IT. And not too many people know how to use IT equipment or laptop”.
-Male veterinarian ID6
In addition, IDIs further elaborated on training resources accessibility with insights on how higher training cost could lower preference for MOT or vice versa.
“Because most times when you are organizing physical training for participants, you are limited by funds. Sometimes you can only pick what you can afford but with the virtual, you can, you can take as many as you need to”.
-Male veterinarian ID2
Training characteristics
IDIs added self-efficacy for MOT as some of the factors that could be associated with preference for MOT among public health workers. They expressed their concerns on the differences in self-efficacy of public health workers across area, age, and sex.
“…because they are learned, they can operate the gadget. And, at least they have the basic tools like some have the computer or the handsets that are that can be used to access some of this virtual training”.
-Female public health specialist ID4
Training environment
IDIs expanded knowledge on how external environment might affect preference for MOT. IDIs revealed that public health workers who have more work obligations are likely to have preference for MOT.
“If you have an individual that is so, so tied up with personal work, that particular individual may prefer to do an online program. Then if you have someone that has a little bit time on his hand, they would prefer to do a kind of physical stuff”.
-Female veterinarian ID3
MOT acceptability
Quantitative
Of the 231 public health workers, a population estimate of 95.99% (95% CI= 93.79-98.18) found MOT as an acceptable training modality. The MOT acceptability rate varied by country, from as high as 100% in Benin, Cote d’Ivoire, Ghana, Liberia, Mali, Niger, and Senegal to 77.78% in Cabo Verde and Guinea-Bissau, but this difference was not statistically significant (p= 0.5257), as shown in Appendix 11 Table 2 and Fig. 2. Quantitative findings showed that work area and age had statistically significant associations with MOT acceptability in both bivariate and multivariate analysis. MOT acceptability was less likely among public health workers in rural areas than those in urban areas (aOR= 0.01; 95% CI= 0.01-0.14). MOT acceptability was less likely among public health workers aged ≤ 29 years (versus 30-39 years, aOR= 0.01; 95% CI= 0.001-0.13) and more likely among 50-59 years (versus 30-39 years, aOR= 32.53; 95% CI= 2.53-418.16), and 40-49 years (versus 30-39 years, aOR= 13.64; 95% CI= 1.35-137.94). [Table 3].
Overall, views from the public health workers interviewed indicated a high acceptability for MOT among public health workers, where six interviewees (85.71%) of a total of seven were in agreements, which was consistent with the result from the survey. IDIs were analysed into training resources accessibility, training characteristics, and training environment themes with their respective meta-inferences (Table 3).
Qualitative
Training resources accessibility
In agreement with the survey findings, IDIs with the public health workers suggested that access to ICT, which is mostly dependent on the work area of a public health worker was one of the training resources accessibility factors that could influence the acceptability for MOT.
Moreover, IDIs further validated training resources accessibility with insights on how higher training cost could lower acceptability for MOT or vice versa. Another issue that many complained about was the instability of electricity in their respective workplaces, which they reported could greatly affect the acceptability of MOT among public health workers in their respective countries.
“Yes, it may be accepted provided the facilities are in place adequately, I know they’re good suggestions for training modalities, but also, like in this country, for example, we have issues of internet. Most of the time we have low bandwidth, and also, we have erratic electricity supply. So those are even some of the factors that would not even allow sometimes those internet-based learning”.
-Male public health specialist ID1
Training characteristics
Unlike the survey findings, IDIs revealed self-efficacy, effort expectancy and performance expectancy for MOT as some of the factors that could be associated with acceptability for MOT among public health workers. They expressed their concerns on the differences in self-efficacy, effort expectancy and performance expectancy of public health workers across area, age, and sex. Of note, one of the public health workers believed that despite these differences, that the extensive use of e-learning during the COVID-19 pandemic could have improved the self-efficacy, effort expectancy and performance expectancy for any e-learning intervention (e.g., MOT) among many public health workers in Africa.
“Well, you know, after 2020 we discovered that we could meet without being physical, and people are already getting used to the fact that you don’t have to attend physical meetings. So, in the workplace so many meetings are being held virtually and we still make headway, we plan, we do meetings, we pass information and things are working. So, I believe that we have come to a place where we know there’s no going back again. Yeah, we cannot go back to the way we used to do things before 2020. So, I believe that’s it would be a good thing”.
-Female veterinarian ID3
Additionally, IDIs further expanded on how the characteristics of MOT could influence its acceptability based on the clarity of its instruction.
“Yes, maybe if instructions also are not clear to those that are to undergo the training, it might influence the issue of acceptability. So, once the instructions on the modalities on how to go about the particular training is made very clear prior to the beginning of the course, I think that there is no problem with that”.
-Male public health specialist ID1
Training environment
IDIs expanded knowledge on how external environment might affect acceptability for MOT. IDIs indicated that public health workers who have more work and/or family obligations are likely to find MOT acceptable, while they also acknowledged the challenge of possible distractions during training.
“So, the first thing is, the kind of work the person does, looking at animal health work, it is mostly field based. So, I think it going to also affect acceptability regardless of the training model. Because it’s possible someone who is taking a self-paced course leaves and goes to the field for weeks to attend to animal health diseases issues, and then when the person returns, they can go over the course again”.
-Male veterinarian ID6
“So, if we look at, the person relationship because at times if one is doing self-paced, the person might want to take that course when they are already at home after work, and everything, and then, maybe at a time to have time for your kids or your wife or husband. That might also affect that learning because they have gone to work from 8 to 5 in the routine hours, and once you take a computer to start going through your course, it might seem to be another thing”.
-Male veterinarian ID6
MOT willingness to use
Quantitative
Of the 231 public health workers, a population estimate of 95.56% (95% CI= 93.78-97.35) were willing to use MOT. The MOT willingness to use rate varied significantly by country (p= <.0001), from as high as 100% in Benin, Cabo Verde, Ghana, Mali, Niger, Senegal, and Sierra Leone to 77.78% in Guinea-Bissau (Appendix 11 Table 3 and Fig. 3). Quantitative findings showed that work area and work experience had statistically significant associations with MOT willingness to use in both bivariate and multivariate analysis. MOT willingness to use was less likely among public health workers in rural areas than those in urban areas (aOR= 0.05; 95% CI= 0.01-0.40). MOT willingness to use was less likely among public health workers with work experience 21-30 years (versus ≤ 10 years, aOR= 0.02; 95% CI= 0.001-0.367) [Table 4].
Overall, opinions from the public health workers interviewed indicated a high willingness to use MOT among public health workers, where six interviewees (85.71%) of a total of seven were in agreements, which was consistent with the result from the survey. IDIs were analysed into training resources accessibility, training characteristics, and training environment themes with their respective meta-inferences (Table 4).
Qualitative
Training resources accessibility
In alignment with the survey findings, IDIs with the public health workers suggested that access to ICT, which is mostly dependent on the work area of a public health worker was one of the training resources accessibility factors that could influence the willingness to use MOT.
Also, IDIs further supported training resources accessibility with insights on how higher training cost could lower willingness to use MOT or vice versa. Another issue that many were worried about was the instability of electricity in their respective workplaces, which they reported could considerably affect the willingness to use MOT among public health workers in their respective countries.
“I will say, take the example of Ministry of Health, the Ministry of Health in all services they have the internet connection, so already, it is not necessarily given money when I say motivation, it is not giving money, it’s making sure that the person has an internet connection because when you ask someone the connection remains expensive in Africa because you can buy internet worth 60 gigabytes when you talk about a distance course, it’s going to be a platform to download videos etc”.
-Female public health specialist ID7
Training characteristics
In contrast to the survey findings, IDIs revealed training relevance and training content as some of the factors that could be associated with willingness to use MOT among public health workers. They emphasized that MOT would have to be relevant to public health workers in terms of relevance to their job, or countries, or subregional priority diseases, or topical public health issues, for them to be willing to use it.
“Yeah, I believe they will be willing to participate. Well, if they perceive that this kind of training is going to be beneficial to what do they do in their workplace then they will surely do it”.
-Female veterinarian ID3
More so, IDIs further validated how the characteristics of MOT could influence the willingness of public health workers to use it with based on the quality of its contents. It was many suggestions that public health workers would be willing to use MOT if it contains practice-based teachings with indigenous and contextually feasible practices other than merely textbook standards.
“because I said a lot of countries perhaps do not have their own platforms, but even with those that we often have, it is the design of content that is the issue, and therefore if we have a subregional platform who manages to make adapted content and for different practitioners in all sectors, I think it would be quite innovative and then people will be interested”.
-Female environmentalist ID5
Training environment
IDIs expanded knowledge on how external environment might affect the willingness of public health workers to use MOT. IDIs suggested that public health workers who have more work and/or family obligations are likely to be willing to use MOT, while they also acknowledged the challenge of possible distractions during training.
“…in this country, it is only less than 10% of veterinarians that work in the public or government. Over says 70 to 80% of them work as private individuals, so some of them need time, they need their time. So, moving them around might not be convenient for them. We will be able to have them join you virtually from wherever they are to attend your training, contribute what they need to contribute…”,
-Male veterinarian ID2
Workplace ICT availability
Quantitative
Of the 231 public health workers, a population estimate of 82.09% (95% CI= 77.50-86.68) reported availability of ICT for MOT. The MOT workplace ICT availability rate varied significantly by country (p= 0.0020), from as high as 100% in Senegal to 25% in Mauritania (Appendix 11 Table 4 and Fig. 4). Quantitative findings showed that country, work area, age, sex, discipline, sector, setting, performance expectancy, attitude, and previous e-learning had statistically significant associations with workplace ICT availability for MOT in bivariate analysis, however, only work area remained statistically significant in multivariate analysis. Workplace ICT availability for MOT was more likely among public health workers in rural areas than those in urban areas (aOR= 2.57; 95% CI= 1.22-5.40) [Table 5].
Overall, thoughts from the public health workers interviewed suggested a high workplace ICT availability for MOT among public health workers, where all the seven interviewees (100%) were in agreements, which was consistent with the result from the quantitative survey but highlighted many challenges as well. IDIs were analysed into training resources accessibility, training characteristics, and training environment themes with their respective meta-inferences (Table 5).
Qualitative
Training resources accessibility
IDIs expanded knowledge on training resources accessibility, where it was might pointed out that workplace ICT availability for MOT among public health workers might be based on country and work area, particularly stressing out the issue of internet connectivity. While many believed that a considerable number of public health workers have some access to ICT at their workplaces, they expressed the problem of insufficient internet data bundles and low internet bandwidth. They additionally shared that this problem often challenges their capacity building potential in two major ways. First, they stated that poor internet connectivity often limits their engagements in e-learning, for example, in situations where there was a complete lack of internet services in their workplaces or homes, even when they still had adequate data bundles for internet connectivity. Second, they also mentioned that their lack of access to good internet bandwidth in their countries reduces the effectiveness of e-learning for their capacity building, for example, in instances where they experienced multiple internet disconnections during an ongoing training session.
“Whether it is for example, internet-based, it depends on how much access to internet this particular individual has based on the environment or location, if not, they wouldn’t want to do it based on the experience that we have from conducting trainings. Like in a IDSR, WHO training, we invited a lot of the fieldworkers to participate and attend on scheduled period, but some will register and then may not end up attending the meeting because they didn’t have the facilities available to make them attend. Not that they were not willing to but they because the environment was not feasible for them”.
-Male public health specialist ID1
MOT contextual fit
Quantitative
Overall, the quantitative findings on preference and acceptability of MOT among public health workers from 16 West African countries as extrapolated using the PCoF tool rating guide in Appendix 3, suggests that MOT is of “somewhat contextual fit” among public health workers in West Africa. MOT contextual fit varied by country, from the highest (strong fit) in Benin and Senegal to the lowest (weak fit) in Guinea-Bissau and The Gambia (Table 6 and Figure 3). In the multivariate analysis, only work area and age were found to have statistically significant associations with both MOT preference (area, p= <.0001; age, p= <.0001) and acceptability (area, p= 0.0023; age, p= 0.0009) in Table 2 and Table 3 respectively, which could be inferred as major predictors of MOT contextual fit among public health workers in West Africa. Other factors including sex, attitude, previous e-learning, and workplace internet funding that demonstrated statistical significance in either case of preference or acceptability were considered as minor-moderate predictors of MOT contextual fit.
Qualitative
Qualitative interviews provided insights about electricity and training cost as factors for training resources accessibility; self-efficacy, effort expectancy, performance expectancy, and training instruction clarity as factors for training characteristics; and work area, worker’s age, and work and family obligations as factors for training environment by confirmation or expansion, or discordance with quantitative findings (Table 2 and Table 3).
MOT feasibility
Quantitative
Overall, the quantitative findings on willingness to use and workplace ICT availability for MOT among public health workers from 16 West African countries as extrapolated using the PCoF tool rating guide in Appendix 3, suggests that MOT has “strong feasibility” among public health workers in West Africa. MOT feasibility varied by country, from the highest (strong feasibility) in Ghana, Mali, and Senegal to the lowest (weak feasibility) in Mauritania (Table 7 and Figure 4). In the multivariate analysis, only work area (rural or urban) was found to have statistically significant associations with both MOT willingness to use and workplace ICT availability (MOT willingness to use, p= 0.0092; workplace ICT availability, p= 0.0128) in Table 4 and Table 5 respectively, which could be inferred as a major predictor of MOT feasibility among public health workers in West Africa. Another factor that demonstrated statistical significance in either case of MOT willingness to use or workplace ICT availability was work experience, which was considered as a minor-moderate predictor of MOT feasibility.
Qualitative
Qualitative interviews offered insights about electricity, training cost, internet connectivity, and country as factors for training resource accessibility; training relevance and training content as factors for training characteristics; and work and family obligations as factors for training environment by confirmation or expansion, or discordance with quantitative findings (Table 4 and Table 5).
DISCUSSION
While evidence suggests the increasing use of e-learning for training of public health workers on EPR core competencies given its convenience and cost-effectiveness, research shows that the implementation of these interventions remains a major challenge in Africa, particularly in West Africa, where the need is greatest due to increased epidemic- and pandemic-prone diseases burden and health workers shortage.2,5–7,11,14,27,28,38,39,42–44 Therefore, understanding the contextual fit and feasibility of e-learning for capacity building of public health workers is important to provide baseline evidence that could help improve policies and programs to support their effective uptake for maximum impact on global health security. In this study, we evaluated the contextual fit (with outcomes on preference and acceptability) and feasibility (with outcomes on willingness to use and workplace ICT availability) of MOT among public health workers in 16 West African countries using a mixed-methods design and a novel PCoF tool rating system (Appendix 3). Overall, triangulating the quantitative and qualitative findings, we found that MOT is of “somewhat” contextual fit and has a “strong feasibility” for implementation among the public health workforce in a resource-limited setting like West Africa. More so, we observed variability in these findings across countries and some associated factors, which may in part be due to differences in the structural determinants such as economic strength, technology, and policies of the countries that affect the living or working conditions and behavioural choices of the population.
In this study, the “somewhat” contextual fit for MOT was explained by a combined ranking of MOT preference rate of 29.6% (ranked as moderate) and MOT acceptability rate of 96.0% (ranked as high), which were both found to be significantly associated with work area and age and were inferred as major predictors of contextual fit. In addition, we found other factors that were determined as minor-moderate predictors, including sex, attitude towards ICT, previous e-learning, and workplace internet funding that demonstrated statistical significance in either case of preference or acceptability. These findings are consistent with results reported in Africa and comparable to results from other regions of the world.12,16,45–47 We further found that many public health workers attributed the contextual factors associated with preference and acceptability of MOT to factors around training resources accessibility (electricity and training cost); training characteristics (self-efficacy, effort expectancy, performance expectancy, and training instruction clarity); and training environment (family and work obligations) that could have influenced the MOT contextual fit and feasibility ratings demonstrated in this study, especially for the suboptimal level of MOT preference observed. Specific insights shared by many of them included, for example, interruptions in e-learning due to erratic electricity, or how public health workers with higher work obligations are likely to prefer e-learning than other modalities and are unable to effectively use it due to distractions from work. Overall, our findings support the body of knowledge on preference and acceptability of e-learning, where similar associations have been established, but remains inconclusive.12,16,45–47 This variability in findings may be because of differences in settings, target populations, existing country social policies, study sample size, and research methodology.
Specifically, in our study we found that the likelihoods of preference and acceptability of MOT were lower for public health workers in rural areas when compared to those in urban areas, which could be attributed to lower access to ICT resources and differences in inadequate digital literacy that have been reported in similar settings.45,48,49 Contrary to general knowledge, we found that those who are young (≤ 29 years) were more likely to have preference for MOT and less likely to accept MOT compared to public health workers aged 30-39 years. This finding provided new insights that having preference for a digital solution might not correlate with the acceptability of such intervention due to several factors. One of the explanations for this, could be that, while young public health workers demonstrated a higher preference for MOT maybe because of its added benefits (e.g., convenience, cost-effectiveness) and their well-known technological proficiency with ICT tools, they might have found MOT unacceptable based on disagreement with the form in which e-learning interventions are being currently designed (e.g., lack of context-specific content) and delivered (e.g., poor interactivity and engagement) in the African setting. Although, this finding was observed among the young subpopulation, this issue is also relevant for the different age groups in the public health workforce with implications on low uptake and poor fidelity of e-learning interventions that contribute to its ineffective scale up for meaningful public health impact. This finding suggests the need for more research among young public health workers to better understand the factors associated with their acceptability for e-learning to improve its adaptation and implementation in West Africa and other similar settings. This is important given evidence of employment shift to younger people worldwide, in which young people aged 15-29 years account for 19.2%-28% of the health and social workforce in LMICs, which is largely driven by the increasing youth populations and retirement of aging workers.50–52 Notably, is the rising state of this trend in Africa, where youths account for 65% of its total population.53 Further, these findings emphasize the importance of using a robust methodology like the PCoF tool that concurrently measures both preference and acceptability of an EBI (e.g., MOT) to assess its contextual fit other than basing this assessment on either preference or acceptability, as it has been historically practiced. In addressing these geographic and age gaps in e-learning implementation among public health workers, there is a need for more proactive multisectoral leadership, aligned investments, and evidence-informed policies (e.g., rural- and youth-responsive digital policies) to shift the implementation of e-learning from a state of “siloed learning initiatives” to “integrated learning systems” that are supported by relevant national, regional and global infrastructures for its sustainability and health systems strengthening.
These findings on preference and acceptability of MOT align with existing evidence, for example, a meta-analysis by Dedeilia and colleagues that was performed to assess the modalities of training among health workers between 2020 and 2022 across six WHO regions showed that 29.7% of African health workers preferred e-learning, which is similar to 29.6% reported in this study.12 On the other hand, our finding on MOT acceptability with a rate of 96.0% is slightly higher but comparable to 90.5% reported from a scoping review on training modalities among public health workers, with included articles between 2000-2019 and from Africa.16 Some of the reasons that may provide explanation for the observed increase in the acceptability of MOT, include first, the increased use of e-learning during the COVID-19 pandemic due to social distancing measures (e.g., lockdown) that restricted the participation of public health workers in the conventional F2F training modality, where it is likely that the self-efficacy, effort expectancy, and performance expectancy of public health workers towards e-learning could have increased as a result. Second, is the possibility that the inherent characteristics of MOT with multiple options, including a training that incorporates a combination of synchronous and asynchronous online methods with a wide range of ICT-enabled approaches such as facilitated learning and social media-based learning might be perceived by public health workers as more user-friendly and responsive to their busy work schedules, thus generating more acceptability. Nevertheless, our results shed additional light on the complexity associated with population decision making towards acceptability and use of e-learning in the African context. Practically, we believe this study underscores the importance of engaging potential end users of any EBI for better understanding of the contextual issues to inform culturally appropriate and people-centered policies for public health workforce capacity building, improved job performance, and return on investment in the areas of health, education, and economic growth.
Similar to MOT contextual fit, the “strong feasibility” of MOT was explained by a combined ranking of MOT willingness to use rate of 95.6% (ranked as high) and workplace ICT availability rate of 82.1% (ranked as high), which were both found to be significantly associated with work area and was inferred as a major predictor of feasibility. Work experience was determined as a minor-moderate predictor given that it demonstrated statistical significance in either case of MOT willingness to use or workplace ICT availability. These findings agree with what were reported in previous studies.12,16,45–47 We further identified that many public health workers attributed the contextual factors associated with MOT willingness to use and workplace ICT availability among public health workers to themes around training resources accessibility (electricity, training cost, and country); training characteristics (training relevance, and training content); and training environment (family and work obligations) that could have influenced our results. Specific views reported by many of them included, for example, their inaccessibility to ICT resources for e-learning despite their willingness to use it.
Our findings on willingness to use MOT is higher than 49.5% reported in the same meta-analysis by Dedeilia and colleagues.12 Comparable to the observed increase in acceptability for e-learning as found in our study, we argue that improvement in the self-efficacy and perhaps the performance expectancy of public health workers towards e-learning from sustained use during the COVID-19 pandemic might be some of the factors responsible for this increase. In the same vein, this reason might be attributed to the high rate of workplace ICT availability observed in our study probably as a tangible benefit from the increasing investments in digital technology, which may have been driven by the need to keep public health workers educated despite the pandemic, including those in rural areas. In addition, our study showed that MOT contextual fit varied by country, from the highest (strong fit) in Benin and Senegal to the lowest (weak fit) in Guinea-Bissau and The Gambia. This variability may be attributed to differences in the economic power of public health workers in these countries to access to ICT personally or in their workplaces, where a report in 2018 indicated higher gross domestic product (GDP) per capital in Benin ($2,220) and Senegal ($2,617) versus Guinea-Bissau ($1,500) and The Gambia ($1,882).54
Another possible explanation for this variance could be the difference in digital literacy skills among public health workers as proximate effects of workplace and/or national digital policies in these countries. In fact, according to a World Bank report in 2019, Benin was said to have received a grant of $100 million to expand its digital technology services with a particular focus on rural areas in addition to the existence of national digital policies in the country as well as in Senegal.54–56 Whereas for MOT feasibility, we found Ghana, Mali, and Senegal to have strong feasibility, and a weak feasibility in Mauritania. Similarly, from the economic perspective, evidence suggests that GDP per capital is not only high in the countries with strong feasibility (Ghana, $4,267; Mali, $1,667; and Senegal, $2,617), but digital technology investments are high as well.54,56,57 For instance, Mali was said to have launched its 5G network in 2022, which could mean better internet connectivity and improved preference or acceptability of MOT among its public health workforce.57 In summary, these findings highlight the need for equity-focused policies to increase investments in digital solutions like MOT using a “whole-of-government” approach to bridge geographic and age disparities, plus existing economic and digital gaps for improved learning outcomes among public health workers for global health security. An example of these approaches could be by establishing transparent and collaborative partnerships between the public health sector, relevant non-health sectors (e.g., telecommunication, private institutions) and end users (public health workers) to co-design, co-deliver, and co-manage digital platforms for effective and efficient learning. Lastly, our findings provide baseline evidence to inform the real-world implementation and potential scale up of MOT and related e-learning interventions in West Africa and other relevant settings. See Box 1 for details.
Strengths and limitations
Our study has some strengths. First, to our knowledge, this is the first subregional study that assessed contextual fit and feasibility of an e-learning intervention in all the West African countries among professionally, culturally, and linguistically diverse public health workforce population. Second, our study used a mixed-methods design and novel methodology, both of which accounted for robust explanatory variables and the complexity of any EBI implementation at the population and setting levels. Third, we performed statistical weighting at the country level using data from a 2018 WHO report on health workforce in the African region to make our results more subregionally representative.32 Fourth, we used SAS PROC Survey methodology that accounted for the study design and clustering to reduce analytical bias from inaccurate standard errors estimation.
Our study has some limitations. First, there is a possibility of selection bias due to lack of complete public health workforce database, in which we were unable to apply a random sampling approach and public health workers that chose to participate in this study might have had a greater interest and opinion in the topic, which could have led to the overestimation of our outcome variables. Another possibility for selection bias is from the low participation of public health workers from rural areas, but our finding with a rural-urban ratio of 1:2 is consistent with what is obtainable in most physical surveys. Second, our findings could have been limited by information bias due to our inability to provide explanations to any participants that might need further clarifications to better answer the survey questionnaire given that the quantitative survey in study was conducted online, but this was limited with the design of our questionnaire in simple languages. Third, despite statistical weighting, some countries had low participation in the survey despite efforts being made to promote widespread national participation through emails, social media, official websites, and newsletter of our subregional networks, including the WAHO, the Africa CDC, and the AFENET. Fourth, response rate could not be estimated and adjusted for as a result of anonymity of online survey data collected through emails and the impossibility to determine a sampling frame from responses collected via social media. While the rate of non-response could not be ascertained nor baseline characteristics of responders and non-responders be compared due to our survey design and sampling limitations, the effect of a possible response bias is likely to be low given that our sample was weighted, and the responses are likely to be missing at random. Fifth, our study could not account for social desirability response bias, whereby participants prefer to select the best answer over the true answer. Sixth, there was lack of post-stratification weights for all relevant population characteristics (e.g., age, sex) due to lack of data from our reference population, which could have resulted in residual bias, nonetheless, the country variable is considered to be highly correlated to our study outcomes based on how differences in culture, national priorities, and economic strength are likely to influence acceptability and use of EBIs. Seventh, we had a low IDIs sample size because of non-availability of participants and time constraints and we were unable to accommodate participants from Portuguese speaking countries in the IDIs due to language barrier among the research team, which could have resulted in unbalanced perspectives, but given some similarity in culture with French and English-speaking countries, our findings could be said to be representative. Eight, we had only one public health worker from the environment sector that volunteered to participate in the IDIs, and most interviewees were working in the government and academia as at the time of the interview. However, a sufficient number of them reported work experiences that span the breadth and length of private sector health institutions and non-governmental organizations. Ninth, our IDIs lacked representation of public health workers from the rural areas. This is because all the EPR focal persons that were invited for the interviews were all from urban areas as at the time of this study and only routinely interfaced with their colleagues in rural areas. Hence, this inadequacy could have generated non-representative perspectives due to possible systematic differences in the baseline characteristics and experiences between the public health workers from urban and rural areas. Tenth, due to a scarcity of data on e-learning contextual fit and feasibility outcomes with a rating method like our study, an explicit interpretation of our findings with other studies was impossible, but our interpretation with each study outcome’ constructs provided some insights.
CONCLUSIONS
The study findings suggest that MOT has some contextual fit and is strongly feasible for capacity building among public health workers in under-resourced settings like West Africa, but substantial geographic and age disparities exist, as well as other issues around training resources accessibility, training characteristics, and training environment that could limit its effective implementation and potential health impact. Thus, building a standardized and integrated system for e-learning using a “whole-of-government” approach is warranted to address these disparities for maximized impact. The findings and the methodology demonstrated from this study could help managers, trainers and policymakers in the prioritization, adaptation, and scale up of e-learning as well as other digital solutions among the public health workforce for strengthened digital learning systems in our technologically advancing world, with a particular focus on settings with weak contextual fit and weak feasibility, and underserved populations, including rural and young workers.
Acknowledgements
We are grateful to the emergency preparedness and response focal persons and all public health workers that participated in the study.
Ethics statement
This study was approved by the Emory University Institutional Review Board, and the West African Health Organization (WAHO) provided institutional approval for the conduct of the study. All participants provided informed consent prior to the quantitative survey and qualitative interviews, including the permission to have the interviews audio-recorded.
Data availability
The data underlying this article are available at https://doi.org/10.6084/m9.figshare.24654486.v8.
Funding
No funding to declare.
Authorship contributions
KOO and SM led the conceptualization and design of this study. LSS, VKL, and CO contributed to the conceptualization and provided critical suggestions for the design of this study. KOO, LSS, VKL, SA, MAA, and SM supported the data collection for surveys. KOO conducted quantitative data analysis, verified by SM. KOO and LSS conducted qualitative interviews and data analysis. KOO, LSS, VL, and SM had full access to the data. KOO wrote the manuscript draft. LSS, VKL, and CO made edits to the draft. SA, SK, CH, TN, MAA, and SM performed critical review and provided suggestions for the manuscript writing. All authors read and approved the submission of the finalized version of the manuscript for publication.
Disclosure of interest
The authors completed the ICMJE Disclosure of Interest Form (available upon request from the corresponding author) and disclose no relevant interests.
Additional material
Additional information is provided in the online supplementary document (appendix).
Correspondence to:
Kehinde Olawale Ogunyemi
Hubert Department of Global Health
Rollins School of Public Health
Emory University
1518 Clifton Road, NE
Atlanta, Georgia 30322
USA
ogunyemikehinde89@gmail.com

_amo.jpeg)
_among_.jpeg)


_amo.jpeg)
_among_.jpeg)