INTRODUCTION
Comorbidity refers to the co-occurrence of two or more medical conditions in an individual; these conditions may develop independently but can be linked through chance occurrence, shared risk factors, or one condition arising as a complication of another.1 Comorbidities are frequently chronic and significantly influence an individual’s health outcomes, clinical management, and financial burden.2 COVID-19 and cholera stand as two formidable challenges confronting low- and middle-income nations across Africa and Asia.1,3 Emerging from different origins, COVID-19, stemming from the SARS-CoV-2 virus, first appeared in Wuhan, China, in December 2019, swiftly evolving into a global pandemic.3 It primarily spreads through respiratory droplets expelled during coughing, sneezing, or talking.4
Cholera, caused by the bacterium Vibrio cholerae, is an acute diarrheal disease that has caused significant morbidity and mortality worldwide, particularly in regions with inadequate sanitation,5 resulting from consuming contaminated food or water.6 Since its first documented outbreak in 1817, cholera has persisted as a recurring public health threat, with multiple pandemics claiming countless lives worldwide.7 Despite their distinct origins, COVID-19 and cholera share several notable parallels. Both diseases are considered disruptive forces, originating in Asia before spreading globally.4 Moreover, neither ailment is entirely novel, with human coronaviruses and the original O1 cholera strain recognized as illnesses associated with significant immunity in previously exposed populations.4 While COVID-19 continues to dominate global health agendas, cholera maintains its endemic status in numerous countries, with Africa accounting for a significant portion of reported cases.8 The emergence of the COVID-19 pandemic has further complicated the landscape of cholera outbreaks, particularly in regions already grappling with endemic transmission. Reports of cholera outbreaks in countries such as Ethiopia and Sudan have surfaced concurrently with the COVID-19 era.8 The prevalence of cholera epidemics is often linked to factors such as overpopulation, inadequate sanitation, and poverty, which are exacerbated during times of crisis.8 However, amidst the redirection of resources and strained healthcare systems to combat COVID-19, data on cholera outbreaks in many African nations remain scarce and uncertain. In Asia, cholera remains a persistent concern in various regions, including Afghanistan, Malawi, South Africa, Uganda, and Iraq.4,9 The intersection of cholera outbreaks with the COVID-19 pandemic has placed immense strain on healthcare systems, exacerbating existing challenges.10 In Iraq, where healthcare infrastructure was already weakened by ongoing conflicts, the confirmation of cholera cases further complicates an already dire situation.10 Similarly, in countries like Pakistan and Bangladesh, the prevalence of cholera has surged alongside the COVID-19 pandemic, overwhelming already strained healthcare systems.10,11
The concept of comorbidity adds another layer of complexity to the interplay between cholera and COVID-19. Factors such as socioeconomic status, access to healthcare, and demographic characteristics significantly influence the risk of comorbidities in affected populations.12,13 For instance, populations in low-income settings are more likely to experience severe outcomes due to limited access to healthcare and sanitation facilities.14 Therefore, Individuals with comorbidities face heightened risks of adverse health outcomes, underscoring the importance of tailored care and preventive measures.15 Research has shown that socioeconomic status influences both the risk of infection and the effectiveness of disease management strategies.16
Moreover, the comorbidity of cholera and COVID-19 poses unique challenges in regions where both diseases are prevalent, necessitating targeted interventions to mitigate risks and improve overall health outcomes.17,18 Demographic factors, including age, population density, and ethnicity, further influence the comorbidity of cholera and COVID-19.19 Older individuals are particularly vulnerable to comorbidities, increasing their risk of severe outcomes if exposed to both diseases.19 To fully comprehend the compounded effects of COVID-19 and cholera, it is essential to consider how socioeconomic and demographic variables contribute to the overall disease burden. Improved sanitation and healthcare infrastructure are crucial for mitigating the impact of these diseases. Similarly, population density, urbanization, and mobility contribute to the transmission of both cholera and COVID-19, amplifying the risk of comorbidities in affected communities.3 Addressing these complex interactions requires multifaceted approaches aimed at enhancing healthcare access, promoting awareness, and addressing underlying socioeconomic determinants.20,21 Therefore, the coexistence of COVID-19 and cholera presents multifaceted challenges for affected regions in Asia and Africa. Efforts to prevent and control both diseases must consider their intersecting impacts on populations, healthcare systems, and economies. In summary, the interaction between COVID-19 and cholera highlights the need for targeted public health strategies that address both immediate and underlying factors. Ensuring access to clean water, improving sanitation, and strengthening healthcare systems are vital for managing these diseases effectively.
This work reviews the current state of knowledge on COVID-19 and cholera comorbidity in Africa and Asia and aims to provide healthcare providers, public health providers, and policymakers with the information needed to develop and implement effective interventions to reduce the burden of these diseases. We aimed to answer the research question: What is the impact of the COVID-19 pandemic on the epidemiology, prevention, and control strategies of cholera outbreaks in endemic regions of Asia and Africa?
METHODS
Protocol registration
This systematic review and meta-analysis were conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines for its analyses and synthesis (Figure 1). The detailed plan of our protocol is published and registered with the National Institute for Health and Care Research (NIHR) International Prospective Register of Systematic Reviews (PROSPERO) (registration ID: CRD42023485040).
Data sources
We executed an exhaustive and systematic search across multiple electronic databases to ensure the comprehensive identification of pertinent studies. The selected databases included PubMed, Embase, Web of Science, Scopus, the Cochrane Library, and Google Scholar. This wide-ranging approach was adopted to encompass a diverse array of scholarly publications across the fields of cholera and COVID-19.
Search strategies
The search strategy we used was meticulously designed using a combination of Medical Subject Headings (MeSH) terms and free-text keywords. This strategy was tailored to maximize the retrieval of relevant studies. Specifically, we employed the following Boolean query: (“cholera”[MeSH Terms] OR “cholera”[All Fields]) AND (“sars-cov-2”[MeSH Terms] OR “sars-cov-2”[All Fields] OR “covid”[All Fields] OR “covid-19”[MeSH Terms] OR “covid-19”[All Fields]). This structured search string was devised to capture the literature pertaining to the comorbidity of Cholera and SARS-CoV-2 and its prevalence in Africa and Asia.
Inclusion criteria
We used the participants, interventions, comparisons, and outcomes (PICO) model to frame the study topic.
P (Population): Studies conducted in endemic regions, specifically Africa and Asia, were considered for inclusion. This ensures that the research is directly relevant to regions where cholera is prevalent. Focusing on endemic regions is crucial for understanding the unique challenges and interactions between cholera and COVID-19 in these areas.
I (Intervention): Studies that address the impact of COVID-19 on healthcare systems and cholera management were included. This encompasses research investigating how the COVID-19 pandemic has caused an increase or decrease in the prevalence of cholera. Understanding the impact of COVID-19 on healthcare systems, especially in managing endemic diseases such as cholera, is critical for effective response and mitigation strategies.
C (Comparison): Studies that compare cholera management and outcomes during the COVID-19 pandemic with periods outside the pandemic or with different interventions during the pandemic were included. These studies provide insights into how cholera response and management strategies have been adapted in the context of the pandemic. Eligible comparators included different time periods (pre-pandemic vs. during pandemic), different geographical locations within the endemic regions, and different healthcare interventions applied during the pandemic.
O (Outcome): Studies that measured the prevalence and incidence of cholera during and beyond the COVID-19 pandemic were included. These studies provide essential data on the trends and dynamics of cholera cases in the context of the pandemic. This criterion helps to assess the impact of the COVID-19 pandemic on the prevalence and incidence of cholera, providing valuable insights for public health interventions.
Other inclusion criteria are as follows:
Study Type: Cohort studies, case‒control studies, cross-sectional studies, randomized
controlled trials, and mixed-methods research were considered for inclusion. These study designs provide diverse and robust evidence for understanding the comorbidity of cholera and COVID-19. The inclusion of various study types ensures a comprehensive analysis of the comorbidity and its implications for healthcare systems.
Publication Year: We considered studies published within the last 10 years (2013 to 2023). This timeframe encompasses both the pre-COVID-19 and post-COVID-19 periods, offering a comprehensive view of cholera and COVID-19 dynamics. This criterion ensures that the review captures the most recent and relevant literature, allowing for an up-to-date understanding of the comorbidity.
Publication Status: We considered only the full text; peer-reviewed published articles were considered for inclusion. This criterion ensures the inclusion of high-quality, rigorously evaluated research. Including only peer-reviewed articles helps maintain the quality and reliability of the evidence base, ensuring that the systematic review is based on robust and validated research.
Language: Only studies published in English were considered for inclusion. This criterion allowed us to efficiently review the selected literature. Limiting the review to English-language publications ensures that the research team can thoroughly evaluate and extract relevant information from the selected studies.
Data extraction
First, a preliminary literature search of the selected academic databases (PubMed, Embase, Web of Science, Scopus, the Cochrane Library, and Google Scholar) was performed to identify all relevant publications on cholera and COVID-19 comorbidity among children and adults in Africa and Asia. Four authors worked on the same dataset and reviewed the titles and abstracts independently to identify studies that met the eligibility (inclusion and exclusion) criteria. In cases where there was disagreement between two of the initial reviewers, a third author was consulted to resolve the conflict. This process was invoked in 10-15 instances to ensure consistency and validity in the selection process. To further validate the selection process, a kappa statistic was calculated to measure the inter-rater agreement among the reviewers. For the included studies that were found to be eligible, the following information was extracted: the name of the author(s), year, country, study design, study population, study settings, sample size (total number of cases or participants analyzed in the study), number of participants (number of individuals enrolled in the study), intervention, outcome, and results obtained using a designed data collection form. The full abstract-based search procedure is depicted in Figure 2, together with the use of eligibility criteria (inclusion and exclusion criteria). Duplicates were identified and excluded at this stage.
Quality assessment
The quality of each publication was assessed using the Critical Appraisal Skills Programme (CASP) checklist for systematic reviews, which consists of 10 questions designed to evaluate the validity, results, and applicability of the studies (CASP, 2018). Each study was evaluated based on questions such as whether the review addressed a clearly focused question, whether the authors looked for the right type of papers, whether all important and relevant studies were included, whether the quality of the included studies was sufficiently assessed, whether it was reasonable to combine the results of the review, what the overall results of the review were, the precision of the results, the applicability of the results to the local population, whether all important outcomes were considered, and whether the benefits were worth the harms and costs. Each question was answered with “yes,” “no,” or “can’t tell,” with comments provided to explain the reasoning. The maximum score for each study was 10 points, categorized as follows: good quality (7–10 points), moderate quality (4–6 points), and low quality (1–3 points). Those that met all or most of the criteria with minimal risk of bias were classified as good quality. Studies that met some criteria but had some risks of bias were categorized as moderate quality. Finally, studies that met few criteria and had a high risk of bias were deemed low quality. Two investigators independently reviewed and scored the studies, with discrepancies resolved through discussion with a third reviewer. This process ensured a rigorous assessment of the study quality. The CASP checklist can be accessed at.22
Meta-analysis
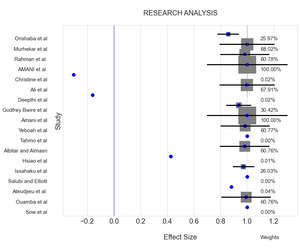
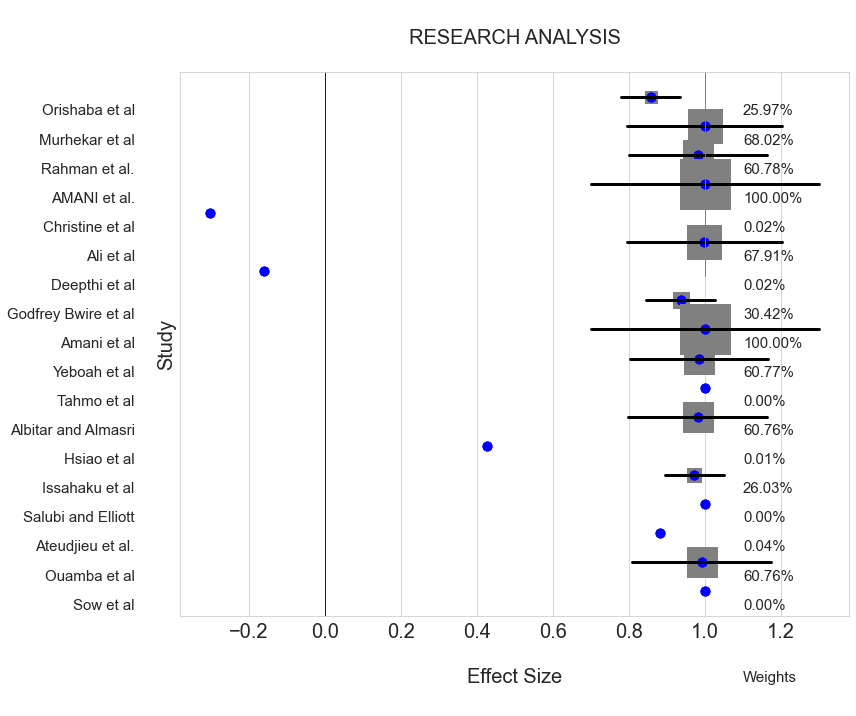
For the meta-analysis, Python and the Pandas library were used to compile and preprocess the data, after which the data were organized for analysis, as shown in Figure 2. A Python-based statistical analysis tool (NumPy) was used to summarize the data and reveal the central patterns in the data prior to computing descriptive statistics such as the mean and standard deviation. Cohen’s d, a measure of effect size, was used to determine the significant difference between one group or intervention and another. This enabled a uniform comparison of the efficiency of diverse techniques across numerous investigations. The Python package (Matplotlib and Seaborn) was used to create visualizations in the form of heatmaps, bar plots, and forest plots.
In summary, the methodology employed in this study involved a rigorous search strategy across multiple databases, clearly defined inclusion and exclusion criteria, and a structured process for study selection and quality assessment.
RESULTS
Search Result and Study Selection Process
After a first search with the combinations of descriptors selected, 642 articles were identified through an electronic database. After the exclusion of the 24 duplicate articles and the analysis of the 629 titles and abstracts, 101 articles were remaining for a full assessment for eligibility. Finally, 83 articles were excluded, and 18 articles were included in the final analysis. All the studies were published in English. Figure 1 shows the flowchart of the research that shows how this selection was performed.
Characteristics of Included Studies
The studies (n=18) described cases of cholera during and post-COVID-19 era, including the prevalence, rate of transmission, history of cholera, clinical diagnosis and disease outcomes. The included studies varied in design, population, and geographic location, but all focused on the comorbidity of COVID-19 and cholera. Included studies used methodologies such as cross-sectional surveys, cohort studies, and case-control studies, examining populations from various countries in Africa and Asia. Table 1 shows the overall characteristics of the included studies showing a total subject of 17,367,836 from 5-64 years old. The COVID-19 pandemic presented both hurdles and opportunities for controlling and preventing cholera with the problems of cholera being evident as a result of dehydration and dryness which can lead to death sometimes.
The Hurdles Associated with the Co-infection
Compared to COVID-19, cholera is a disease that has existed for over three decades with several ongoing preventive measures and treatments. Studies showed that the COVID-19 pandemic may have had a negative impact on the cholera outbreak. For example, it was recorded that the cholera epidemic first appeared in Nigeria in 1972 and of all cholera outbreaks, the worst cholera outbreak was recorded in 2021 (the era of COVID-19), with 111,062 suspected cases across the country, of which 3.5% of the recorded cases resulted in death.30 One of the main hurdles that was identified across the studies is the mode of transmission of cholera and COVID-19. Person-to-person transmission; while COVID-19 can be transmitted in close range to another person, cholera can only be possible through coming in contact with contaminated faeces or food of the infected host.23,25 Water insecurity is another identified hurdle associated with the co-infection.3,23–25,27,33,34,36 Massive open-field defecation among community members or labourers can infect water and, in some cases, the cities or villages only have one source of water for the entire community to share. This suggests that the population were devoid of safe and clean drinking water which may have promoted the increase in the number of cholera cases. Additionally, it was discovered that most people living in rural areas experience food insecurity, which is defined as going without food at least once over the previous three months, all year
long. For patients to treat cholera, 67% of inpatients and 44% of outpatients borrowed money from their churches, families, neighbors, bosses, or the village chief to pay for their medical care, food, or transportation.32 The financial burden also plays a significant role in jeopardizing the COVID-19 situation as the government and healthcare management can’t bear the financial cost to use an alternative for vaccinating the population via mobile means rather than fixed post.3 This can be connected to evidence from a study conducted in Uganda, results documented several bad; food handling practices in the Natapar Kocuc village market had the potential to promote the spread of cholera and other foodborne infections within the communities.23 Kousseri Health District (located in a rural area) did not have many personnel trained in surveillance, with 33.3% observed during the evaluation and one of the health facilities in Mada Health District did not have a nurse.35
The Opportunities Associated with the Co-infection
WASH (Water, Sanitation and Hygiene): WASH intervention was found to be effective in reducing cholera and diarrhea prevalence for the household members of diarrhea patients and this approach serves to reduce diarrheal diseases in cholera hotspots in the developing areas.29,32,38,39 Health Promotion, Vaccination, Sensitization and Education: Educating the public about a particular health condition or disease is an important contribution to the prevention of diseases. Educational interventions were shown to help make healthy choices to maintain good health and achieve a very good quality of life.23,26,29,36 The social media is the second-most popular source of information on cholera after schools and colleges, which represents 31.7% of the population.31 In Ghana, the extended knowledge of the COVID-19 model (E-KCM) that was employed showed that the average COVID-19 knowledge scores were close to 70%, indicating that many of the surveyed respondents had a reasonable level of knowledge about infectious diseases and the COVID- 19 pandemic with over 20% of the population willing to adhere to the safe health guidelines, which also support that district with higher literacy rates had a lower risk of cholera.27,29
Meta Analysis
As shown in Figure 2, a weight was developed for each author’s work based on their sample size and quality assessment score using Cohen’s d. A second computation based on the demographics covered by their work was done, to show the variations in contribution. The meta-analysis showed that COVID-19 and cholera co-infection and co-morbidity in Africa and Asia are strongly positively correlated with 95% CI (0.80, 0.99). The meta-analysis results showed a consistent pattern of increased cholera outbreaks in regions heavily impacted by COVID-19. These findings are in line with previous research that highlights the vulnerability of low-income regions to multiple infectious diseases during a pandemic.8,11 The review discussed how the current findings compare and contrast with earlier studies, emphasizing the need for ongoing surveillance and research. So also, these findings are consistent with previous research that has established a strong link between poverty or low socio-economic status and infectious diseases.40 Several outliers were identified in the meta-analysis, primarily from studies with small sample sizes or those conducted in regions with unique health challenges. Sensitivity analyses were performed to assess the impact of these outliers, revealing that their exclusion did not significantly alter the overall findings. This robustness suggests that the observed associations are reliable and not unduly influenced by anomalous data points.
In summary, this systematic review and meta-analysis employed a rigorous methodology, including a comprehensive search strategy, detailed inclusion and exclusion criteria, and robust statistical analysis. The results indicate a significant association between socioeconomic factors and the comorbidity of COVID-19 and cholera, highlighting the need for targeted public health interventions in low-resource settings. The identification of publication bias and outliers was addressed through sensitivity analyses, ensuring the reliability of the findings.
Publication Bias
Publication bias was assessed using Egger’s publication bias plot with results shown in Figure 3. The precision of the studies (X axis) was plotted against standard normal deviate (SND) which shows the effect sizes of the studies in terms of their standard deviations. The data points represent the studies included in the meta-analysis positioned according to its precision and effect size, with the fitted line being the regression line from Egger’s test for publication bias, where a significant intercept suggests the presence of publication bias.
In our analysis, the data points appear somewhat symmetrically distributed around the fitted line suggesting that there might not be a strong publication bias, but the outliers need to be considered. Moreover, there are a few points (e.g., “Ateudjieu et al” and “Orishaba et al”) that deviate significantly from the fitted line, which could indicate some degree of bias.
DISCUSSION
COVID-19 emerged in late 2019 and caused a global pandemic due to a constant increase in the number of confirmed cases and deaths.41 There have been reports of higher cholera outbreaks with diverse investigations suggesting an association between COVID-19 and cholera.23,28 The COVID-19 pandemic resulted in over 10,000,000 deaths worldwide, and during this period, there were over 400,000 cases of cholera.42 However, there is still limited scientific information about COVID-19 co-infection with cholera. Therefore, to understand the epidemiological standpoint, this study summarizes the cases of cholera outbreaks during and post-COVID-19 era. We assessed 18 studies. Our principal findings reveal that most of the population that suffer most from the pandemic are in poor settings with little or no health infrastructure aid. Another relevant result is that inadequate access to clean water is a huge risk factor that poses a threat to the healthcare system. Seven African nations, including Nigeria, reported cholera outbreaks during the COVID-19 pandemic, which exacerbated problems with the already overburdened healthcare systems.37 Comparing the findings of Uganda with Nigeria, the results showed that the status of the COVID-19 pandemic in Nigeria worsened the cholera situation, suggesting the presence of other factors along with the COVID-19 pandemic impacting the cholera outbreak.23,34 Additionally, a large proportion of people in Malawi, especially those living in rural areas, are easily prone to frequent flood disasters.32 Therefore, in tackling water insecurity, the implementation of WASH is one of the most effective and long-term solutions, which is beneficial in combating both diseases, thereby following the recommended standard of WASH and restriction in public gatherings and other preventive measures applied to promote awareness and advocacy on COVID-19 as well, suggesting an opportunity for averting the cholera outbreak.
On health education and vaccination, it was found that the COVID-19 outbreak affected both the acceptability of the cholera vaccine and the COVID-19 vaccine. In Cameroon, the overall oral cholera vaccination (OCV) coverage was low28 due to the misconceptions about vaccines that are being shared on social media, also with the lack of adequate gadgets to identify vaccination teams.26,28,29,36 Additionally, the educational tool that was administered in the early COVID-19 pandemic posed a challenge to the majority of the population thereby affecting the vaccine acceptability.31 However, with appropriate healthcare trainers and educators during the vaccination exercise, the targeted population was able to learn and maintain all other interventions for cholera response including WASH.23 Therefore, in this era of the cholera outbreak and COVID-19, it is necessary to address WASH intervention, vaccination, and health education with utmost importance to reverse the damage caused by misinformation about vaccines and re-educate on the benefits of vaccination and sanitation.
The findings from our meta-analysis highlight the interplay between the burden of COVID-19 and cholera, particularly in resource-limited settings. For example, the analysis showed a statistically significant correlation between the prevalence of cholera and the burden of COVID-19 in countries like Nigeria and Uganda, which is consistent with the narrative findings from the included studies.
However, the present study has some limitations. First, the reliance on published studies means there is potential for publication bias. Second, the heterogeneity in the study designs and settings of the included studies may introduce variability that affects the generalizability of the findings. Finally, data gaps and inconsistencies in reporting cholera and COVID-19 cases could impact the accuracy of the findings. These limitations underscores the need for more standardized and comprehensive data collection methods in future primary research.
CONCLUSIONS AND RECOMMENDATIONS
This systematic review spotlights the compounded challenges faced in controlling cholera outbreaks amidst the COVID-19 pandemic, particularly in low-resource settings. The dual burden has strained healthcare systems, highlighting the need for integrated and comprehensive strategies involving both government and local authorities. Vaccination campaigns, public awareness, and robust surveillance mechanisms are essential components in mitigating the impacts of these concurrent health crises. The analysis revealed that inadequate healthcare infrastructure and water insecurity are significant risk factors exacerbating the dual burden of cholera and COVID-19. Addressing these issues requires targeted interventions and sustained efforts. Specific actionable recommendations include enhanced vaccination campaigns, where governments should implement targeted vaccination efforts for both cholera and COVID-19, ensuring accessibility in remote and underserved areas. This can be achieved through the deployment of mobile vaccination units and the involvement of community health workers to increase coverage and acceptance. Additionally, public awareness programs are crucial. Initiating comprehensive education efforts to dispel misinformation about vaccines and promote the benefits of both cholera and COVID-19 vaccinations is necessary. Utilizing local media, social platforms, and community leaders can help reach a broader audience and enhance public trust in vaccination efforts. Moreover, strengthening WASH interventions is essential. Investing in water, sanitation, and hygiene infrastructure to reduce waterborne disease transmission is critical. Ensuring a clean water supply and adequate sanitation facilities in high-risk areas can significantly mitigate the spread of cholera. Furthermore, robust surveillance systems should be developed and maintained to monitor and swiftly respond to outbreaks. Integrating cholera and COVID-19 surveillance can lead to more effective outbreak management and resource allocation.
Finally, supportive healthcare infrastructure is necessary. Increasing investment in healthcare facilities to better handle concurrent outbreaks is vital. This includes equipping healthcare facilities with the necessary resources and training healthcare workers in managing co-infections. By enhancing the capacity of healthcare systems, it becomes possible to provide timely and effective treatment, reducing the overall burden of disease. Through these specific and actionable recommendations, comprehensive strategies can be developed to control cholera outbreaks amid the COVID-19 pandemic and beyond.
Further research is needed to understand the interplay between cholera and COVID-19, particularly in different epidemiological settings. Detailed studies on the effectiveness of combined intervention strategies are essential to identify the most efficient approaches for simultaneous management of both diseases. Longitudinal studies should be conducted to assess the long-term impacts of co-infections on public health, providing valuable insights into the persistent effects and potential complications arising from dual outbreaks. Additionally, research on innovative technologies and methodologies for improving vaccine delivery and acceptance is crucial to enhance immunization efforts and overcome barriers to vaccination. Studies focusing on the socioeconomic impacts of dual outbreaks and effective policy responses are also needed to develop targeted interventions that address the broader consequences of these concurrent health crises.
Data availability
The data supporting the findings of this study are available within the article and its supplementary materials.
Funding
This research received no external funding.
Authorship contributions
Conceptualization: O.C.A. O.O.O.; figures: O.O.O., O.C.A. and O.F.; writing, review and editing of the drafts and final versions of the manuscript: O.C.A., O.O.O., I. I., V.A.A., and O.F. All authors have read and agreed to the published version of the manuscript.
Disclosure of interest
The authors completed the ICMJE Disclosure of Interest Form (available upon request from the corresponding author) and disclose no relevant interests.
Correspondence to
Dr. Olalekan Chris Akinsulie
Washington State University
1650 NE Valley Rd, Pullman WA 99163,
United States of America
olasulie@gmail.com