Human Immune Deficiency Virus (HIV) remains the leading cause of death of more than 30 million people around the globe. Despite all innovations in care, HIV still causes fatal and lifelong impacts on an individual’s health.1 Furthermore, the global burden of HIV among young people between the ages of 15 to 19 is 17 per 100,000 individuals, and for the age group 20 to 24, it is reported as 24 per 100,000 individuals.2 Regionally, Africa has a larger burden of HIV among young people, where mostly young women are infected compared to young men. In Europe and the United States, this shift is more towards men, and the common reason that prevails among young people is Men having Sex with Men (MSM). Whereas in Asia, young Injection Drug Users (IDUs). are commonly seen as the most affected by HIV.3 The young age group is fragile and naive due to biological origin and developmental stages. However, the prevalence of HIV among young people is seen widely due to developmental and environmental sources.4
HIV in Pakistan has grown since its first documentation over thirty years ago, showcasing several patterns throughout these decades.5 According to the United Nations (UN) report, Pakistan had up to 120000 cases of HIV reported in 2009.6 Pakistan is also one of those countries where the prevalence of HIV is documented due to several common etiologies, including unsafe sex practices, IDUs, and utilization of unscreened blood products.5,7 In a study, the total number calculated of People Living with HIV (PLH). in Pakistan is documented to be 94000 in different population groups.8 Ministry of Health Pakistan and the National AIDS Control Program (NACP)'s joint report of 2005 displayed that HIV among Female Sex Workers (FSW). in Karachi was 2%, and in Lahore, it was 1%.9 In 2006, a study conducted in two cities of Punjab showed the prevalence of HIV between 10 to 12% among the total population.10 Another study in the same year reported an 8% HIV prevalence in Larkana.11 Leading towards 2007, research in Quetta showcased that the prevalence of HIV among IDUs is around 24% of the total population.12
In 2019, most children were infected by an HIV outbreak in Pakistan, in the Ratodero area of Larkana District, Sindh. The reports suggest that the common reasons for this outbreak were unscreened blood transfusions, needle reuse, and male circumcision through septic equipment. According to World Health Organization (WHO)., among the overall population screened in Ratodero, more than 700 were infected with the virus, and many children and young people were included in this count.13
According to the NACP website and the records, an estimated 2 20,000 people are living with HIV, and among those, 53,713 are registered under the NACP. Of the registered PLHs, 33,007 receive treatment as Anti-Retroviral Therapy (ART). from 51 centers across the country.14
Young people constitute around 60% of Pakistan’s population.15 The age group is considered productive and has a significant role in improving countries’ status of indicators in health and education. The age group also has a potential contribution to the economic stability of their families and the country. Through the international report, we could understand that 2/7 of new cases reported every time regarding HIV in 2019 were of young people between the age group of 15 to 24 years old.2,3,16 These ratios and numbers are distinctly not recorded as for Pakistan but in the present condition. From the recording of the outbreak, we can conclude that among all these reported, Pakistan must be included as well. Also, the findings shared by WHO estimated that children of 0 to 14 years old and young women over 15 years of age constitute around 2000 cases in Pakistan.8,17,18
Apart from the reasons and potential causes listed in the incident of Ratodero, Sindh, there is furthermore discussion across the world regarding the root causes of the reasons HIV increases among young people. These causes included reckless behaviors, early sexual contact, older sexual partners, lack of comprehensive sexuality education, and no use of condoms while involved in any sexual conduct.19 Furthermore, the Young People Living with HIV (YPLH) has a close connection with vulnerability, which also increases the disease’s prevalence and refrains them from accessing healthcare for health improvement and seeking timely treatment. Approximately 90% of Asian YPLH are categorized among the following vulnerable groups: MSM, transgender, prisoners, sex workers, and drug users.20 Most of the studies available globally have no proper identifications of age groups and less inclusion of young people. In comparison, studies of Pakistan related to HIV/AIDS are very limited to accommodate and specific to the young age group. We aim to explore the challenges in healthcare access for young people living with HIV/AIDS.
Methods
In this review, we conducted an extensive literature review using a systematic approach to examine peer-reviewed literature related to challenges in healthcare access for young people living with HIV. In this review we have use constructs modified from frameworks on healthcare access put forth by Penchansky and Thomas (1981) and Levesque et al. (2013) to comprehend data-driven dimensions of challenges that directly impact the access to healthcare services for YPLH (Figure 1).
The literature search was conducted using scholarly databases, including PubMed, Medline, Google Scholar, Cochrane, and Science Direct, from January 1, 2008, to February 23, 2023. The review was completed in one month time by March 30th, 2023. Dissertations, full-text articles, abstracts, and bibliographies in articles that met inclusion criteria were selected. We captured our three main categories of a similar population set using the terms youth, adolescents, young people with HIV/AIDS between ages 12-29, and the challenges they face in accessing health care services. The keywords used for this basic literature search included youth, adolescents, young people living with HIV, AIDS, HIV care, Healthcare access, and healthcare access challenges.
To avoid the risk of error and systematic bias at any stage of our review, we incorporated explicit and systematic methods to undertake a comprehensive search that identifies the maximum number of eligible primary sources.
We applied our search criteria oand identified 35 records. All records were exported to an EndNote database for inclusion/exclusion evaluation (Table 1).
Data collection
Two authors independently screened abstracts to determine relevance. Full paper copies were reviewed against the inclusion criteria. The findings were extracted by both authors and compared. We also conducted a three-stage screening process, starting with a title review, then an abstract review, and ending with a full-text article review. Articles were included if they addressed challenges to healthcare access faced by young people with HIV. For this search, editorials and opinion pieces were excluded. In our title review stage, three authors (SS, WQ, ZA) independently reviewed the journal article titles to determine whether they were relevant or irrelevant.
RESULTS
Search results
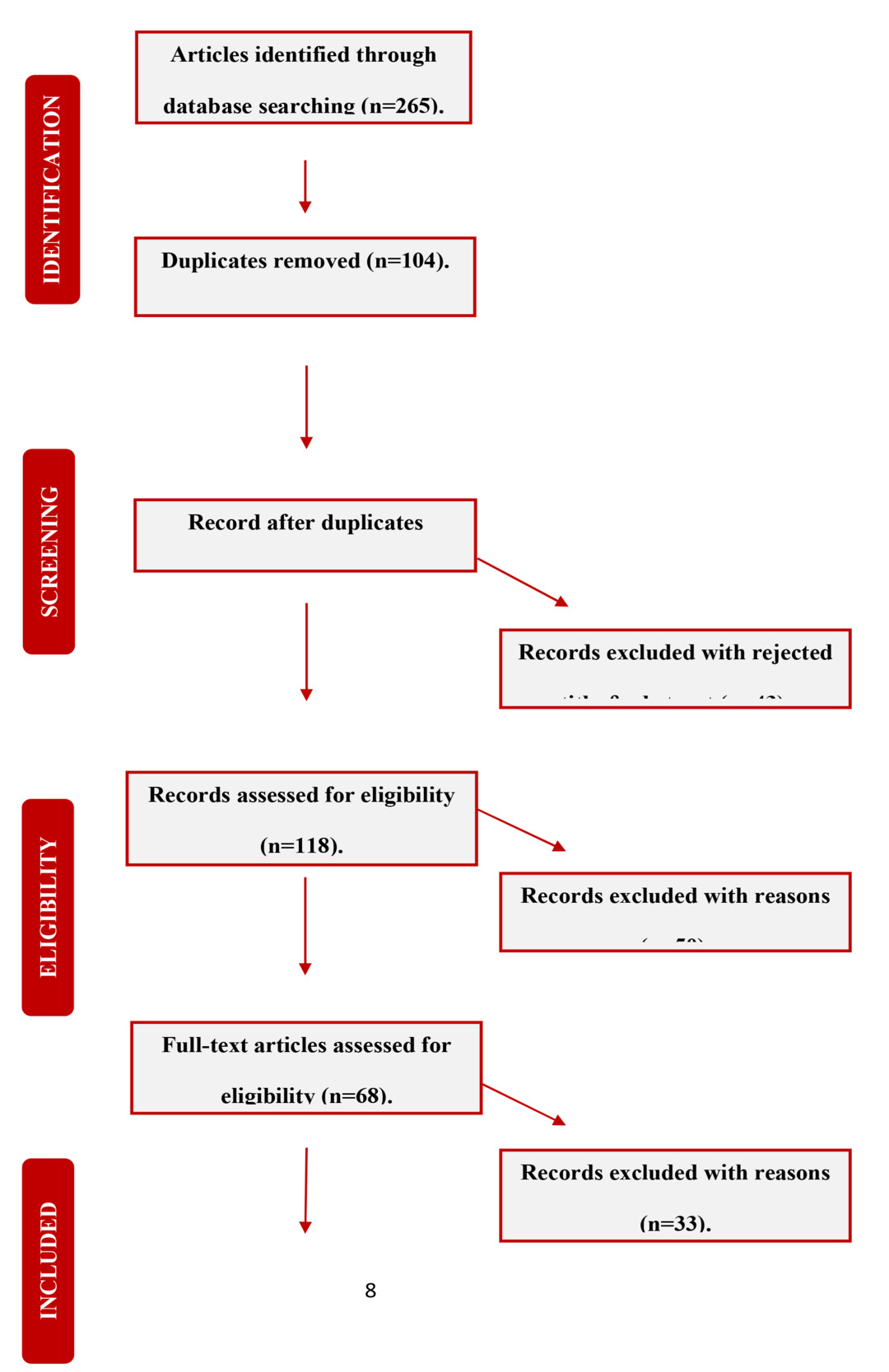
An initial database search revealed 265 articles from all four search engines. 104 Duplicates were removed, followed by the screening of 161 articles based on the title of this review. Forty-three were excluded based on the title and abstract of the articles. During the process where the consensus of finalizing articles was difficult the supervisor and final author’s (TSA)'s advice was undertaken. In our second stage, the authors independently screened the abstracts of the remaining 118 articles and determined that 50 still unmet eligibility criteria. The remaining 68 full-text articles were found eligible. Upon further reviewing them, we excluded 33 records that were not aligned with our inclusion criteria. Hence 35 articles were included as they were deemed to be relevant to the title and fully met the inclusion criteria. The PRISMA diagram describes the complete selection process stepwise (Figure 2).
Main findings
The reviewers then developed a data abstraction table and specified descriptive statistics (Table 2).
This representation gave us a detailed snapshot of the included articles according to their year of publication, author, study method, study setting, and a brief description. Once abstraction was complete, the team met to review all of the data and developed themes into categories for challenges to healthcare access for young people with HIV/AIDS. Themes were consolidated according to the dimensions described in (Figure 1).
Based on the data that emerged from articles, we formulated major categories of challenges (e.g., stigma, disclosure, travel distance, financial challenges, knowledge gaps, etc.), following which categorization description of findings and conclusions were derived from the relevant studies under each category (Table 3). Using this abstraction tool helped with the independent abstraction of information from 35 articles with merged concepts under the common category of information, each finalizing the list of challenges to healthcare access by young people. Authors were instructed to highlight any themes not captured by the abstraction tool; however, no other key themes emerged.
DISCUSSION
The Analysis based results of the literature is further documented as categories and the discussion is based on connecting the research objective.
Challenges to HIV health care access
There has been a presence of rich literature concerning the subject area across the global regions. However, the exploration among populations chosen or taken differed in age groups. This literature review not only provides insights from studies about healthcare access concerning HIV-positive individuals but also provides the connection of challenges with the age group of youth, which is the primary concern group of this study.
According to this basic literature search, multiple factors have been seen as challenges for PLH regarding accessing healthcare (Table 3). These challenges include travel and commuting, financial and educational lacking, lack of health insurance, vulnerability, stigma, and religious values. Despite a wider clarity, there is less understanding through research studies that there are significant other challenges that can be age-relevant or specified for young people only. As per the condition of HIV in Pakistan, there are various studies available from Pakistan that share insights and shed light on the situation, condition, beliefs, and knowledge of HIV, but there is still a larger scope to explore the experiences of YPLH regarding healthcare access and its relevant components, concerning the
potentially productive and the most prevailing youth group in the country living and fighting with the disease. The hindrances to accessing ART may be linked with the elements that stop PLWHA from seeking care after being diagnosed with HIV. Individuals who seek HIV care may be impacted negatively by other factors such as differences in health setup, providers’ experiences, and characteristics of the patients.21
a) Affordability
Financial challenges
Four studies from a systemic review conducted in east Africa revealed financial constraints and poverty as significant challenges in adhering to HIV treatment. This also includes the transport fares that are necessary for taking up medical treatment. This study also mentioned the difficulties in continuing education in school due to financial difficulties.49
Individuals who develop AIDS infection experience high costs of medical expenses. The physiological and psychological status of individuals with good incomes can bear the costs and also receive help from families.23
Many of the studies which focus on YPLH facing challenges to access healthcare comprise young transgender persons as a population due to their vulnerability to acquiring the virus as a result of risky sexual behaviors and practices. A group of twenty-eight transgender persons, mostly transgender women, in Spain were included in a study to know the opportunities to improve healthcare issues. This group was major of YPLH, comprising of median age of 28 years old. Twenty-two out of 28 participants reported that accessing healthcare is difficult and challenging in Madrid. One eye-opening fact that also needs an important consideration was that no one of these participants had health insurance to support healthcare expenditure. This becomes another important factor making healthcare access further challenging.24
Alike these two studies, another study in Nigeria shares that traveling and lack of health insurance both are common challenges for PLH to access healthcare.
This study has no specification regarding age group. However, the majority of the participants were females coming from low socioeconomic and low educational statuses. Which also serves as an indirect factor in healthcare access for PLH. In this situation, the Nigerian PLH must rely mostly on public healthcare services whose quality is not up to standards. This also brings inequity in the healthcare system, as the less educated and less privileged in terms of money cannot access healthcare.25
b) Acceptability
i. Disclosure
A study conducted in Pakistan recruited 287 HIV/AIDS patients and documented that the stigma and disclosure level is higher in females than males. It also mentioned that treatment-seeking is delayed in males exposing them to increased death rates.25 Challenges associated with disclosure are multilayered. The individuals who are infected sexually carry guilt and often find it difficult to confront their families, and the youth who are affected perinatally usually blame their parents in such situations. The fear of disclosure to parents or guardians often limits access to healthcare services. There is a need to address the issues concerning confidentiality.4
ii. Stigma/discrimination
Stigma remains another top-notch hurdle for accessing healthcare. The pieces of evidence come from both Islamic and non-Islamic countries. Countries like Iran have healthcare stigma associated with religious values, and countries like India have stigmatized nature related to the disease present itself. It is seen in India that general healthcare access is comparatively less challenging than access to HIV-related healthcare.32 This situation is also similar in Europe, where studies from countries like Ireland disseminate that adherence to HIV treatment by the PLH decreased timely, only because of healthcare stigma.33
The behaviors of healthcare providers have been reported in various studies. Though many documented attitudes as positive and respectful, on the other hand, many document communication problems between the two, which serves as a major barrier in providing care to these individuals.57
Individuals perceive HIV/AIDS as incurable due to improper communication by healthcare providers.58 In accessing HIV care, high costs, medication accessibility, confidentiality, and stigma pose great challenges.34–36 The quality of care is affected by stigma and discrimination by healthcare providers. The ME data shows that even in countries with supportive programs, stigma, and discrimination were present among healthcare staff. These factors affected adherence to medication and increased risky behaviors.37 In the sample of PWID, stigma was common, and 62% reported stigma from healthcare providers. In rural PWID, stigma impacted health and high-risk injecting behaviors.38
iii. Social support
There is very little explored in the literature about social support when it comes to HIV. Especially for young people, social support is common, as it remains available for young people in general without any HIV status. However, most social support is associated with psychological well-being but is not majorly explored regarding its connection with healthcare. A basic view can be seen documented, which directs toward the continuity of healthcare and compliance with medicine when encouragement is received by family or related people.59 Families are unaware, and they couldn’t provide the support which is usually required for YPLH. However, an African study has shown that people of color reported stereotypical attitudes in families, and that impacted social support in general for people with HIV.34 There is also evidence in the literature that an increase in conflict among families is documented because of HIV diagnosis in young people at home, and that impacts the relationship and social support.60 A study from China reports that spouses and families are the major support systems, and lower scores of social support are seen in all sorts of HIV-positive people. The major burden is on men and unmarried individuals. There is less evidence of ethnic, religious, and gender-based communities’ support for young people in this regard. However, observations reveal that in Pakistan and India, many CBOs and people within communities like transgender and MSM communities formulate groups for social support to specific young people fighting HIV.
In comparison with domestic norm people social support is lower in people with HIV/Aids.23 Care-seeking behavior is affected by a lack of social support and financial support, which ultimately results in missed clinic appointments for these individuals.39
In addition, research shows that HIV-related stigma and discrimination can serve as a major barrier to the uptake of specialized HIV care.61,62 Due to fears of social exclusion, some PLHIV cannot choose treatment facilities in their communities and maintain anonymity, even with extra time and cost.31
c) Availability
Lack of education
One of the main reasons for poor retention of HIV care and adherence is the lack of education. A Study from Zambia reports a lack of knowledge regarding the medication that they are taking. It also states that improvement in adherence to care can be achieved with education.50
Many studies document that HIV/AIDS was not heard by 23% of the students, whereas 56% believe it to be mosquito-borne. Moreover, it was also associated with the notion that it is a disease affecting non-Muslims.27 An Iranian study reported a good amount of knowledge among medical students, which accounted for 37%, and 23% of non-medical students had awareness about AIDS.28 In India, HIV knowledge was found to be 36% among adult males, whereas only 20% of females were aware of HIV. In the USA, HIV transmission & safe sex knowledge were found to be low in young adults.55
The growing cases in rural areas pose some serious gaps where HIV prevention knowledge is reported at 5.2% and 4.2%, respectively.43 In Pakistan, there is insufficient awareness and knowledge among young adults.58
d) Approachability
Travel distance
Another interesting study conducted in Uganda on the quantitative approach focused on around 447 individuals revealed that there are no healthcare services nearby the residential location of the village, and PLH has to additionally travel for 2 kilometers to access the healthcare facility. The study was conducted on individuals who were of age 18 and above, which includes a good number of young household residents. They have to pay more to access care compared to HIV-negative individuals.29
Linkage to HIV care also decreased significantly with distance to the clinic. In the TasP trial, 40% of people were diagnosed with HIV by HBHCT and had not been in HIV care.30
In the Ahafo-Ano South district, Ghana, healthcare utilization is affected by long distances and travel time. The same is found in Nigeria and Zambia, where access to HIV clinics is associated with a facility located at far distances. The public transportation issues, high cost of travel, and poor road-long travel reflect the structural barriers in sub-Saharan African countries.31
Limitations
The literature search was limited to English language articles from the last 15 years and run using PubMed, Google Scholar, Medline, science direct & Cochrane. It is likely that relevant articles are missing from this review that was published in other languages and indexed in databases besides PubMed (such as CINAHL, Web of Science, PsycINFO, Embase, etc.). The inclusion of those missing articles could have added more information on challenges to healthcare access. In addition, this review was designed to answer a specific question and highlight various challenges to healthcare access for young people with HIV. The articles discussing recommendations or solutions were examined but not retrieved and included. Our literature review did not focus on recommendations, policies, or strategies to address healthcare access issues for this population, which might provide additional evidence to rectify the gap in service delivery not mentioned in this paper. Another review latest measures to overcome these challenges and upgrade healthcare access for young people would be needed. Because the review aimed to examine challenges in general rather than comparing the challenges by country, we are unable to present comparisons across countries. Further research would be needed to answer this question.
CONCLUSIONS
To conclude, it was determined that HIV-stigma and its effects complicate the difficulties of living with HIV/AIDS, necessitating interventions for YPLH’s wellbeing to comprehend and confront the stigma. Decentralization of HIV care at government hospitals and the expansion of ART sites in rural areas will cut down on travel time and transportation expenses while ensuring that all YPLH have access to healthcare services. The way that PLH use healthcare services is seen to be hampered by the discriminatory or improper attitudes and practices of healthcare workers at healthcare institutions. These difficulties may be caused by structural reasons like social pressure, personal & societal ignorance about HIV, restricted access to HIV prophylaxis, and regulatory impediments. The findings imply that to facilitate the readily accessible HIV care services for youth it is vital to increase society’s and healthcare professionals’ awareness of HIV at every level.
Ethical Approval and Consent to participate
Not Applicable
Consent to publish
Not Applicable
Funding
No funding
Availability of data and materials
Available to corresponding author on request.
Author’s contribution
SSm - Conceptualization, Writing original draft & Reviewing.
WQ & ZA- Methodology, Data curation & Writing, Reviewing, and Editing.
TA- Reviewing, Editing and Supervision
Acknowledgement
None
Disclosure of Interest
The authors completed the ICMJE Disclosure of Interest Form (available upon request from the corresponding author) and disclose no relevant interests / declare the following activities and relationships: …" ICMJE declaration forms should be collected and kept by the corresponding author.