Introduction
An estimated 19.3 million new cancer cases (18.1 million excluding nonmelanoma skin cancer) and almost 10.0 million cancer deaths (9.9 million excluding nonmelanoma skin cancers) occurred worldwide in 2020. The global cancer burden is expected to reach 28.4 million cases in 2040, a 47% increase from 2020, with a larger increase in transitioning (64% to 95%) versus transitioned (32% to 56%) countries due to demographic changes, although this increase may be further exacerbated by increasing risk factors associated with globalization and a growing economy.1 In most areas of the world, infectious diseases and other noncommunicable diseases are the main focus, but cancer is becoming an emerging epidemic. In Africa, the burden is increasing due to the increase in life expectancy and population growth. However, this number is underestimated because of the lack and shortage of proper diagnoses of cancer, cancer care, and inadequate data keeping systems.2,3 The majority of these cancers appear to be infection related, which warrants identifying the burden for early preventive measures.4
Globally, the incidence of cancer is fluctuating, and different strategies have been devised to combat it, but the circumstances in China, in this region, have been poor. Low- and middle-income countries are disproportionately affected by cancer, with Africa, Asia, and Central and South America accounting for more than 60% of the cases and 70% of the world’s cancer deaths. In African countries alone, in 2018, there were 811,200 new cancer cases (4.5% of the world total) and 534,000 cancer deaths (7.3% of the world total).2,5
The burden of noncommunicable diseases, including cancer, is increasing in Ethiopia. Cancer is the second leading cause of death in the adult population, accounting for approximately 5.8% of total national mortality.6 According to the population cancer registry in the capital of Addis Ababa, yearly, there are approximately 60,960 cancer cases and over 44,000 deaths in the country. For people under 75 years of age, the risk of being diagnosed with cancer is 11.3%, and the risk of dying from the disease is 9·4%.6,7 Early diagnosis and screening are fundamentally different strategies in terms of resource and infrastructure requirements, as well as overall impact and cost. To effectively implement early detection programs, health planners and policy-makers must be equipped with good data on local/-regional disease burdens (which can be addressed with population-based cancer registries) and sociocultural norms, that can influence the acceptability, feasibility and uptake of services.
The most frequently diagnosed cancer worldwide is female breast cancer, followed by lung and colorectal cancer.1 Breast cancer in women and prostate cancer in men have now become the most commonly diagnosed cancers in many sub-Saharan African countries, replacing cervical and liver cancers.3 However, in every corner of the world, genetic constituents, chemical exposures, lifestyles, infectious diseases, and nutritional components that either increase or prevent cancer may vary. All these variations lead to variations in the pattern of cancer. Therefore, determining the histopathological patterns of cancer is very useful, especially in low-income countries such as Ethiopia, as it may help in the development of plans, provide areas of focus for preventive measures and establish cancer screening programs. The results of this study are also very useful in the planning and management of resources and provide a basis for further in-depth planning and expansion in the area. The aim of this study was to determine the pattern of cancer from pathologic examination samples at GAMBY Teaching General Hospital (GTGH).
Methods
Study Area and Population
GAMBY Teaching General Hospital is one of the largest private hospitals in Ethiopia and is located in northwestern part of the country, the Amhara region, Bahir Dar city, and 572 km from the capital Addis Ababa. The hospital has specialty services, including internal medicine, surgery, pediatrics, gynecology & obstetrics, ophthalmology, orthopedics, etc., with additional subspecialties in neurosurgery, nephrology, and hepatobiliary departments. Currently, it is the leading private teaching and referral hospital in the area, with all-inclusive histopathology and cytology services in its pathology department. The pathology unit is composed of full-time and par-time pathologists and histopathology technicians. In addition to histopathology and fine needle aspiration cytology (FNAC), hematopathology (bone marrow aspiration cytology), fluid cytology, and cervical cancer screening (Pap smear) are services that are also included in the unit. Appropriate and standard methods are followed in sample collection and data recording activities.
Inclusion and Exclusion Criteria
All biopsy and FNAC samples, including incisional and excisional tissue samples with conclusive diagnosis that fulfilled the biopsy request form, were included. All histopathologically confirmed cancer cases during the 5-year period were used to evaluate the cancer distribution. Poorly registered medical records (missing site of tumor, residence, or age) were excluded.
Study Design and Period
A retrospective analysis of pathological examination results recorded from January 1, 2016, to December 30, 2020, was performed with descriptive statistics.
Sample size and sampling
All pathological examination (biopsy and FNAC) result records of patients attending the cancer clinic (pathologic unit) of GTGH from January 1, 2016, to December 30, 2020, were included in the study.
Data collection and analysis
Relevant data, including demographic characteristics, such as age, sex, place of residence, cancer type, diagnosis, treatment type, and pathology results, were extracted from the registry via a data collection checklist. A structured data extraction tool was prepared on the basis of the objective of the study, and important variables, such as sociodemographic characteristics, were included. The data collection process was conducted by physicians and laboratory assistants working in the department, and the extracted data were cross-checked with patient documents by a leading physician to ensure the accuracy of the data. After the data were cleaned with Microsoft Excel, descriptive statistics such as the mean, proportion, percentage, and standard deviation were used to describe the data with respect to the patients’ sociodemographic data and type of cancer. All the collected data were assessed for data quality, completeness, and consistency, and descriptive statistics were generated via SPSS software version 26. All of the patients’ data were available on the registry in the department, and the confirmations of the diagnoses were all made in the department.
Ethical Consideration
Ethical approval was obtained from the Institutional Review Board of GAMBY of Medical and Business College. Since we used a retrospective study of medical records, the IRB of the college waived the requirement for informed consent. A formal letter was written to GTGH to obtain permission for the extraction of data from patient documents. Data were extracted anonymously and kept confidential in the department.
Results
Magnitude of Cancer with Age and Sex
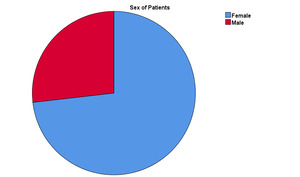
A total of 4320 biopsy and FNAC samples were examined for the detection and identification of cancers from January 1, 2016, to December 30, 2020, over the 5-year period. Among these patients, 895 (20.7%) had confirmed malignancies. A total of 655 (73.2%) of the malignant cases were females, and 240 cases (26.8%) were males, as shown in Figure 1, with a male to female ratio of (1:2.72). The median age of all the patients was 50 years, with a mean age of 49.17±14.94 years, and the age range was from 2-85 years. The mean ages of the females and males were 47.67± 13.36 and 53.19±17.93years, respectively. Children under the age of 15 years accounted for 1.2% of the cancer cases and composed the least affected age group on the basis of our finding, as shown in Table 1. There were fewer confirmed cases among females younger than 15 years than among males. The majority of the confirmed cancer cases were predominantly distributed within the age range of 30-69 years, but the most common age group affected was between 46 and 60 years of age, as shown in Figure 2. The magnitude and distribution of cancers according to sex and age are presented in Table 1.
Distribution of cancer on the basis of anatomical site and histologic type
Among the total cancer cases, the most common cancer was cervical cancer, (31.9%), the second most common cancer was breast cancer, (12.7%), the third most common cancer was nonmelanomatous skin cancer, (11.6%), the fourth most common cancer was primary lymph node cancer (7.7%), and the fifth most common cancer was colon and anorectal cancer, accounting for 5.5% of all cancer cases. Cancer involving the lung, eye and pancreas was among the least common cancers (0.1%, 0.2%, and 0.3% respectively). (Figure 3)
Overall, the most common histologic patterns found were squamous cell carcinoma (48.7%), adenocarcinoma (15.9%), ductal carcinoma (11.8%), non-Hodgkin (6.7%), and papillary ca (4.2%). (Table 2).
Among female patients, the top five cancers in order: included cervical cancer (43.6%), which was by far the most common cancer among females. The mean age of the patients was 50.5+11.4 years, which was between 40 and 60 years. Squamous cell carcinoma was the most commonly reported histological variant (94.7%), and the remaining variant was adenocarcinoma (5.3%). Female breast cancer (14.8%) was the second most common cancer, and the histology findings revealed that ductal carcinoma accounted for 90.7%, mucinous carcinoma accounted for 3.1%, and carcinoma in situ accounted for 3.1%. Tubular and lobular carcinomas were also found but to a much lesser extent. The third most common cancer among females was nonmelanoma skin cancer (8.4%), and the most common histological variant was squamous cell carcinoma (83.6%), with approximately 7.2% basal cell carcinoma and 5.4% dermatofibrosarcoma protuberans. Thyroid cancer (4.6%) was the fourth most common cancer, approximately 83.5% of which was papillary cancer. Follicular cancer accounted for 6.6%, carcinoma in situ accounted for 6.6%, and anaplastic cancer accounted for 3.3%. Malignancies involving the lymph node were the fifth most common cancer (4.3%), 64.3% of which were non-Hodgkin lymphoma, and the remaining (35.7%) were secondary malignancies (ductal carcinoma, squamous cell carcinoma and adenocarcinoma from the surrounding tissues or distant sites). (Table 3)
Among male patients, the top five cancers were nonmelanoma skin cancer (20.4%), of which 73.5% were squamous cell carcinomas, 16.3% were dermatofibrosarcoma protuberans and 6% were basal cell carcinomas. The second most common cancer was lymph node malignancy (17.1%), 92.7% of which were non-Hodgkin lymphoma, 2.4% were Hodgkin lymphoma, and the others were secondary malignancies. Colon and anorectal cancers (10%) were the third most common cancer; 91.7% of them were adenocarcinoma, and the rest were mucinous and squamous cell carcinomas. Bone and soft tissue cancers (8.75%) were the fourth most common cancer, of which 38.1% were sarcoma, 14.3% were osteosarcoma and pleomorphic carcinoma, and 9.5% were chondrosarcoma and squamous cell carcinoma. Male breast cancer was the fifth most common cancer (7.1%), with a male-to-female ratio of 1:5.7, and more than 50% of cases occurred in individuals above age 49. A total of 82.3% of male patients with breast cancer had ductal carcinoma, 11.7% had carcinoma in situ, and 5.8% had mucinous carcinoma. (Table 3)
Discussion
In this study, females accounted for 73.2% of the cancer cases, which was comparable to the figures reported in other studies, such as Addis Ababa (72.8%),7 Gondar (64%),8 Nigeria (59.7%),9 and Malawi (55.9%),10 and this figure also doubled from the prevalence of cancer in men.11 This could be partly because of the higher incidence of sex-based and gynecologic malignancies, such as cervical and breast cancers, in females.
According to GLOBOCAN 2020, in both sexes worldwide, female breast cancer was the most commonly diagnosed cancer (11.7%), followed by lung cancer (11.4%), prostate cancer (7.3%), and nonmelanoma cancer (6.1%).1 The five common cancers in our biopsy were cancers of the cervix (31.9%), breast (12.7%), and samples nonmelanoma skin cancer (11.6%), cancer involving the lymph node (7.7%) and colon and anorectal cancer (5.5%). Our findings are consistent with findings in Kenya.12 However, the differences in standards of living between developed and developing countries, the high prevalence of infection-related cancers, especially cervical cancer, in developing countries, and the increased prevalence of lifestyle risk factors, especially smoking, in developed countries might have contributed to the differences in the pattern of cancer reported in the worldwide data.
Cervical cancer accounted for 31.9% of all cancer cases and 43.6% of all female malignancies, which was similar to the findings of other studies in Malawi,10 Kenya12 and Addis Ababa.13 It is the 7th most common cancer worldwide in both sexes and the 4th most common cancer in females.1 The incidence of cervical cancer is highest in southern, eastern, and western Africa.14 Twenty-nine centers in 12 sub-Saharan countries, including Ethiopia, reported approximately 300 new cases of cervical cancer annually.15 In females; aged15 years and older, the most common cancer was breast cancer (BC), followed by cervical cancer. In the Amhara and Tigray regions of Ethiopia, cervical cancer was found to be the leading cause of cancer.16 Even though the sample size is very small, our study does point to the same conclusion. This could be associated with the high prevalence of HPV infection. Cross-sectional studies have shown that the overall prevalence of any HPV type in the general population of sub-Saharan Africa for women with normal cytology is 21.8%. The prevalence of HPV types 16 and 18 among invasive cervical cancer cases ranges from 43.7% in Senegal to 90.2% in Ethiopia.17 The northern part of the country where the study area is located shows cervical cancer as the most common cancer type, which is not similar to the pattern in other parts of the country or the globe. Bahir Dar is among the few largest cities in this part of the country where many cancer patients visit for confirmatory diagnosis. Although multicentric studies are needed, the results could be the result of poor screening and a higher prevalence of high-risk HPV types in the community, which warrants further studies and vaccinations to prevent death and suffering from such preventable cancer. This result can also be attributed to the prevalence of HIV coinfection among cervical cancer patients in this region, which needs further study and intervention. Our health system should focus on preventive measures, as these measures could be easily. To date, little has been done, especially with respect to vaccination and early screening.
In our study, female breast cancer was the second most common cancer in females (12.7%). Female breast cancer is the most frequently diagnosed cancer worldwide.1 Breast cancer is the most common cancer, constituting 23% of all cancers in regional cancer estimates,11 as well as in studies in Addis Ababa16 and Nigeria.9 It was third (14.3%) next to lymphomas and cervical cancer in a study in another Amhara city of Gondar.8 Although the findings of our study revealed a relatively lower prevalence of cancer than those reported in other regions of the country and across the globe, it still accounts for a significant proportion of cancer epidemiology. Women’s awareness of precancer screening is likely limited, leading to the advanced late-stage presentation of patients, and the presence of only a few mammography centers could be the most important reason for the high prevalence of breast cancer in the region. Since it can be prevented, our health system should focus on providing health education, increasing facilities for reproductive health, and increasing awareness, and mammography services are very important.
Nonmelanoma skin cancer was the third most common cancer in females and the most common cancer in males. Nonmelanoma skin cancer is responsible for more than 1 million new cases (excluding basal cell carcinoma) and 64,000 deaths globally, with incidence rates approximately 2 times higher among men than among women. However, the data in our study revealed a male to female ratio of 1:1.12. It is the most frequently diagnosed cancer in Australia/New Zealand, where the rate is the highest in both men and women worldwide.1 Research conducted in Ethiopia, revealed that NHL was the most common tumor in men, closely followed by squamous carcinoma of the skin, but our study revealed a higher incidence of skin cancer (20.7%) than primary lymph node malignancy (17.1%). Generally, few studies have been published about skin cancer in Africa, Ethiopia and our study area.
This study revealed that primary lymph node malignancies (17.1%) were the second most common malignancy among males and the fifth most common malignancy among female patients. Non-Hodgkin lymphoma was responsible for 544,000 new cases and 260,000 deaths in 2020. The incidence rates are approximately 2-fold higher in transitioned countries than in transitioning countries. The highest incidence rates are found in Australia/New Zealand, North America, and Europe, with Israel and Slovenia ranking first for men and women, respectively.1 The prevalence of Hodgkin lymphoma was 0.4%. Prior to ART, HIV-infected persons had a 25- to 150-fold higher risk of NHL than did the general population. With ART, the risk of NHL remains 11 to 17-fold greater, depending on the lymphoma subtype.15 In our cases, the HIV status of the patients diagnosed with lymph node malignancies was not determined. This finding might reflect its association with oncologic viral infection and a low CD4 count.
Breast cancer in men is a rare disease, accounting for approximately 1% of all breast cancer cases.18 Although the epidemiological literature regarding female breast cancer is extensive, relatively little is known about the etiology of male breast cancer (MBC). A meta-analysis revealed that the male-to-female ratio was markedly greater in Africa, especially in Sub-Saharan countries.19 In this study, the male-to-female ratio was 1:5.7, which was higher than that reported in other studies. Although the total number of male patients was not large, the proportion of male patients with breast cancer was high. In Ethiopia, no studies have been conducted on the risk factors associated with this cancer. Additional studies involving large amounts of data need to be conducted.
The incidence of prostate cancer in our study was only 1.1%, which is probably due to the absence of core needle biopsy for suspected malignancy and the poor habit of sending prostatectomy specimens for clinically benign hyperplasia to the histopathology laboratory. These could be incriminating factors that could lead to incidental findings and small prostatic cancer.
Lung cancer, which is the second most common cancer worldwide,1 is not a frequently diagnosed cancer in our upsetting, possibly due to the low availability of core needles for deep-seated tumors, including those of the lungs and pleura, poor Bronco alveolar lavage techniques, poor pathology services, and a decreased number of subspecialists in the field, which might contributed to the low prevalence of this cancer.
This study was conducted in a private hospital setting, where patients are sent from different parts of the region. The costs of the procedures, the scarce availability of different specialties and subspecialties, and the absence of core needle biopsies to diagnose deep-seated masses are some of the factors that determine the type of specimens we took from patients; this might have affected the types of cancer seen on our routine day-to-day practice. The retrospective nature of the study and the difficulty in including the subsequent outcomes of patients were also additional limitations of the study. Some important risk factors, such as the HIV status of the patient, are missed, which may increase the degree of association with different factors.
In conclusion, this study highlights the cancer burden in the Amhara region. Furthermore, large-scale studies should be performed from population cancer registries to obtain a complete picture of the cancer burden in the region. The prevalence of cancer reported in this study showed varied globally, across Africa, and other regions of the country. Even though the incidence of cancer significantly varies, the histologic findings for each of the common cancers are similar to findings around the world, Africa, and other regions of the country. The absence of subspecialty services, precancerous screenings for cervical, breast and colorectal cancers, inadequate diagnostic imaging, poor service and utilization of vaccination, and poor pathologic services might be some of the reasons associated with the disparities in the prevalence of cancer observed in our study. Even though multicenter study is important for determining the exact prevalence of cancer, this study could be very important for policy makers to understand the gap in minimizing the cancer burden and develop an approach to reduce the cancer burden in the region. The expansion of oncologic services, health education, screening and vaccination services, advancements in diagnostic modalities, and the involvement of the private sector in the management and care of cancer patients are very important health system focuses that should force policy makers to allocate resources accordingly. Those with confirmed cancer cases were linked back to the referring physicians/hospitals or referred to the only cancer treatment center in the town.
Acknowledgments
We are grateful to the GAMBY Private Limited Company for funding this research. We thank the GAMBY Medical and Business College research ethical reviewer committee.
Author Contributions
All authors made a significant contribution to this manuscript in all stages of conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; and gave final approval of the version to be published.
Funding Agent
The funding agent for this study was GAMBY Private Limited Company. The funding body has no influence on the design, data collection, analysis or interpretation of the results. All the things were declared from the funding body.
Availability of Data and Materials
All important data were included in the manuscript, and the corresponding author will share them if additional data are requested.
Competing Interests
The authors declare that they have no potential conflicts of interest.

.png)


.png)